Children of depressed mothers are at increased risk of psychiatric disorders, academic failure, lower social competence, and higher utilization of health services compared with other children (
1–
3). These problems begin early and often persist into adulthood (
4).
Although effective treatments for depression exist, only about half of adults with depression receive treatment (
5); those with low incomes and from minority racial and ethnic groups are significantly less likely to receive treatment (
5–
8). Furthermore, even when depressed parents receive treatment, little is known about the benefit of such treatment for their children. Treating maternal depression may improve child outcomes by improving parent-child relationships, decreasing familial stress, or increasing access to needed services (
2). A review by Gunlicks and Weissman (
9) found that the few existing studies of this topic varied widely in terms of design, characteristics of parents and offspring, and measurement of child outcomes. Of particular importance, only four studies randomly assigned parents to depression treatment in a controlled trial. A majority compared children whose mothers' depression remitted and those whose mothers remained depressed, regardless of the mothers' treatment status.
As an example of the latter type of study, Pilowsky and colleagues (
10) reported that 12 months after the mothers began treatment for depression, children ages seven to 17 whose mothers' depression had remitted had fewer psychiatric symptoms and decreased prevalence of anxiety and depressive disorders than children of mothers whose depression had not remitted. Similarly, Garber and others (
11) found that among children ages seven to 17 over a 22-month period, remission of parental depression was linked with declines in children's self-reported depressive symptoms and improvements in their functioning and competence. Although both of these studies suggested that children improve when their parents' depression improves, the studies' design leaves room for alternative explanations. Specifically, studies that lacked a control group of untreated parents (
10–
12) leave open the possibility that differences in child behavior or the family environment preceded—and perhaps even contributed to—mothers' remission, rather than being a result of remission. The benefits to children of a parent's remission that occurs spontaneously or over a longer period may differ from the benefits produced through effective treatment. A controlled design is also necessary to determine whether a mother's psychotherapy conveys differential benefits to children compared with medication treatment.
To address these concerns, this study examined the effects on children of treatment for maternal depression among women enrolled in a study of evidence-based treatments for depression among low-income women from minority groups (
13). Because of the controlled research design, we were able to assess children's outcomes in relation to their mothers' treatment group assignment and to examine whether children's outcomes were associated with remission of their mothers' depression.
As previously reported, at baseline the children of the depressed mothers enrolled in the study had more emotional and behavior problems and lower social competence and had experienced poorer parenting and more stressful family environments than children of sociodemographically similar mothers who had never been depressed (
14). In this study, we hypothesized that children whose mothers were assigned at random to receive evidence-based depression treatment would have fewer behavior and emotional problems and better adaptive skills at follow-up than children whose mothers were referred to existing community services (most of whom received no treatment).
The experimental design of the treatment study allowed us to determine the effect of mothers' treatment on children's outcomes apart from characteristics that may both predispose mothers to receive treatment and predispose children to better outcomes. Second, because not all women who were offered depression treatment actually remitted and some women who were not assigned to active treatment experienced remission, we examined whether children whose mothers' depression remitted had better outcomes at six-month and 12-month follow-ups than children whose mothers remained depressed.
Methods
Sample
Participants were women enrolled between 1999 and 2002 in a study of the effectiveness of treating depression among low-income women belonging, for the most part, to a minority racial-ethnic group (
13). Mothers with a child ages four to 11 living with them at least 50% of the time and who had a current major depressive disorder were asked to participate in a substudy involving children (
14). Eighty-four who met the criteria were randomly assigned to receive medication (N=27), manualized cognitive-behavioral therapy (CBT) (N=34), or usual care, an active referral to existing community services (N=23). Previous articles described the inclusion and randomization procedures of the depression treatment study (
13) and recruitment and characteristics of the child sample (
14).
As background, for the overall sample of women—mothers and nonmothers—guideline-concordant care (either medication or psychotherapy) was effective in reducing depressive symptoms at six-month and 12-month follow-ups (
13). Medication also resulted in improved social functioning and greater likelihood of symptom remission. Similar results were obtained for the subsample of women in the treatment study who had children ages four to 11—active treatment with medication or psychotherapy resulted in declines in depressive symptoms and improved social role functioning.
At baseline, mothers' mean±SD age was 31.8±6.4. They were primarily African Americans (N=35, 42%) or Latina, first-generation immigrants (N=48, 57%); one (2%) was Caucasian. Almost all (N=82, 98%) were biological mothers. One child from a family was randomly selected for study participation if more than one child was eligible. Forty boys and 44 girls participated (age 6.4±2.0 years). Children with severe learning problems, mental retardation, or other developmental disabilities were excluded from the study sample.
Measures
Sociodemographic characteristics.
Mothers reported their age, race and ethnicity, education, marital status, income, and the child's age, race and ethnicity, and gender.
Remission.
Mothers completed a structured version of the Hamilton Depression Rating Scale (HDRS) (
15) by telephone at baseline and at six-month and 12-month follow-ups. Possible scores on the HDRS range from 0 to 53, with higher scores indicating greater severity of depression. A score of 14 or greater was required for eligibility for the treatment study (
13). At follow-up, remission was defined as an HDRS score <7 and a 50% reduction in the score at baseline.
Child outcomes.
Mothers completed the Behavior Assessment System for Children (BASC) (
16), a reliable, valid rating scale of child behavior and emotional problems and adaptive functioning that provides age- and gender-normed t scores (50±10). The Behavioral Symptoms Index (BSI) of the BASC measures emotional and behavior problems, including depression, anxiety, aggression, hyperactivity, and other disruptive behaviors. The Adaptive Skills Composite (ASC) of the BASC measures social competence and adaptive skills, including prosocial, organizational, and study skills. Possible scores on the BSI and ASC range from 20 to 80, with higher scores indicating more behavior problems or better adaptive skills, respectively; t scores above 70 are considered clinically significant.
Procedures
Recruitment of mothers and children and baseline assessment procedures are described in detail elsewhere (
14). Assessments of children were conducted in participants' homes at baseline and at six-month and 12-month follow-ups. Mothers and children gave written consent or assent using procedures approved by the institutional review boards of the Johns Hopkins Bloomberg School of Public Health and Georgetown University Medical Center. Mothers received $35 for each interview and children received a $10 gift. Interviewers were unaware of the mothers' depression and treatment status. Interviews were completed in Spanish, as needed, by bilingual interviewers.
Data analysis
Following Miranda and colleagues' data analysis strategy (
17), the effect on child outcomes over the 12-month period of mothers' random assignment to treatment was evaluated through a mixed-effects random intercept and random slope repeated-measures analysis, with the BSI and ASC as outcome measures. Mothers' education, marital status, race and ethnicity, and baseline HDRS scores and children's baseline BSI and ASC scores, age, and gender were entered as covariates. Subsequently, the effect of remission of mothers' depression on the same BASC outcome measures was evaluated by using the same analytic approach described above.
Mixed-effects models offer several advantages for analyzing longitudinal data in psychiatric research. The mixed-effects analysis can model change over time at both the group and the individual levels. A separate trend is estimated for each participant, and missing data are augmented by the individual's complete data and information from all other participants in the sample, allowing for the fact that over time, individuals may respond to treatment differently. Finally, this model adjusts for the fact that repeated measures within subjects are correlated, so that estimates of the standard errors are accurate (
18). Mixed-effects models also allow time of measurement to vary for each individual rather than assume that all outcome data were collected at the same time.
Following Miranda and colleagues' methodology (
17), we initially tested for differences among the three randomly assigned groups and separately between the two remission groups in the intercepts, linear slopes, and quadratic slopes. The linear slope is a measure of the continuous change in scores over time, whereas the quadratic slope measures whether the change in child functioning on the BASC was initially steep (at six months) and then leveled out over time (by 12 months). Because quadratic slope was never significant, that term was dropped from the final models shown here.
Results
A total of 68 mother-child pairs completed six-month follow-up interviews, and 63 pairs completed 12-month follow-up interviews, comprising 81% and 75% of the original sample, respectively. Mothers who did or did not complete a follow-up interview did not differ statistically in terms of their baseline age, race and ethnicity, number of children, income, and treatment group assignment. Their children were also comparable in terms of age and gender.
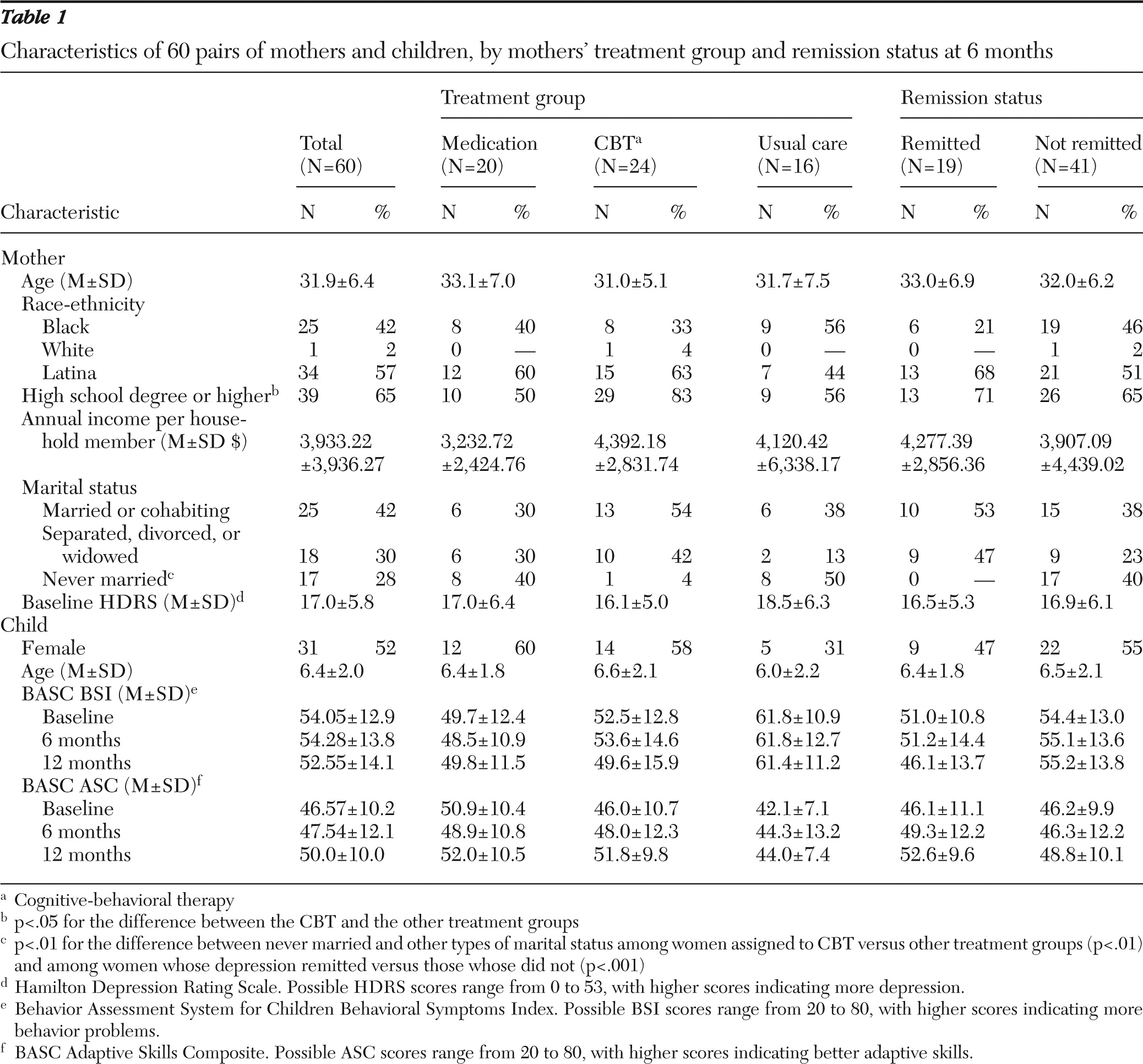
Table 1 provides additional description of the 60 mother-child pairs who completed all three data collection points and constituted the sample for analysis in this study.
As was the case with the women in the main study, despite intensive educational and outreach efforts, many mothers did not receive adequate treatment for their depression (
13). Some treatment was received by 80% (N=16) of those assigned to medication, 83% (N=20) of those assigned to CBT, and none of those assigned to existing community services, or usual care. A minimally therapeutic “dose” of treatment, defined as nine or more weeks of medication or six or more weeks of CBT, was received by 30% (N=6), 29% (N=7), and 0% of the three treatment groups, respectively.
Table 1 shows sociodemographic characteristics, baseline depression levels, and BASC scores for the entire sample and according to treatment group assignment and remission status. These data show baseline differences in education and marital status according to treatment group assignment and differences in marital status according to remission status; thus those variables were controlled in subsequent analyses.
Six- and 12-month intent-to-treat outcomes
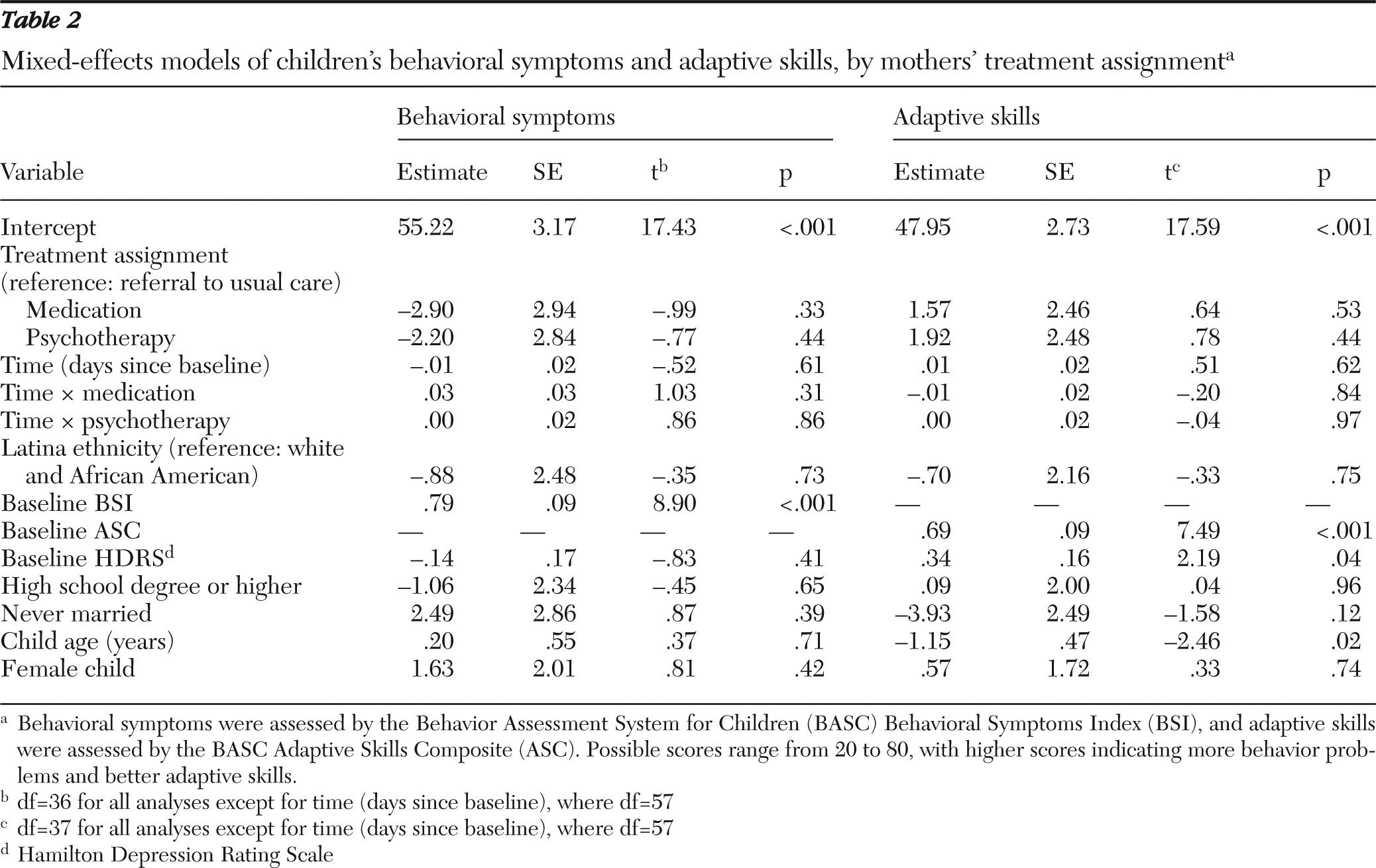
We examined children's behavior problems at six-month and 12-month follow-ups as a function of mothers' random assignment to medication, CBT, or usual care (regardless of actually receiving treatment). The overall multivariate F tests comparing the intercept and linear slope were nonsignificant for medication and for CBT compared with usual care, indicating that treatment did not affect levels or rates of change in child behavior problems when groups were compared within the randomized design (
Table 2).
Among children with similar baseline levels of behavior problems, BSI scores at the six- and 12-month follow-ups were not significantly different in relation to their mother's treatment assignment. Although the effects were nonsignificant, with the exception of BSI scores at the 12-month follow-up of children whose mothers were assigned to the medication group, the direction of all effects indicated fewer behavior problems among children of mothers assigned to active treatment.
Similar models using children's ASC scores as the dependent variable yielded similar results. The overall multivariate F tests comparing the intercept and linear slope were nonsignificant for either medication or CBT compared with usual care, indicating that random assignment to treatment did not affect levels or rates of change in child adaptive skills. Among children with similar baseline levels of adaptive skills, ASC scores at the six- and 12-month follow-ups were not significantly different in relation to their mother's treatment assignment. In all cases, although these differences were nonsignificant, the direction of effects indicated better adaptive skills among children whose mothers were assigned to active treatment.
Six- and 12-month remission analyses
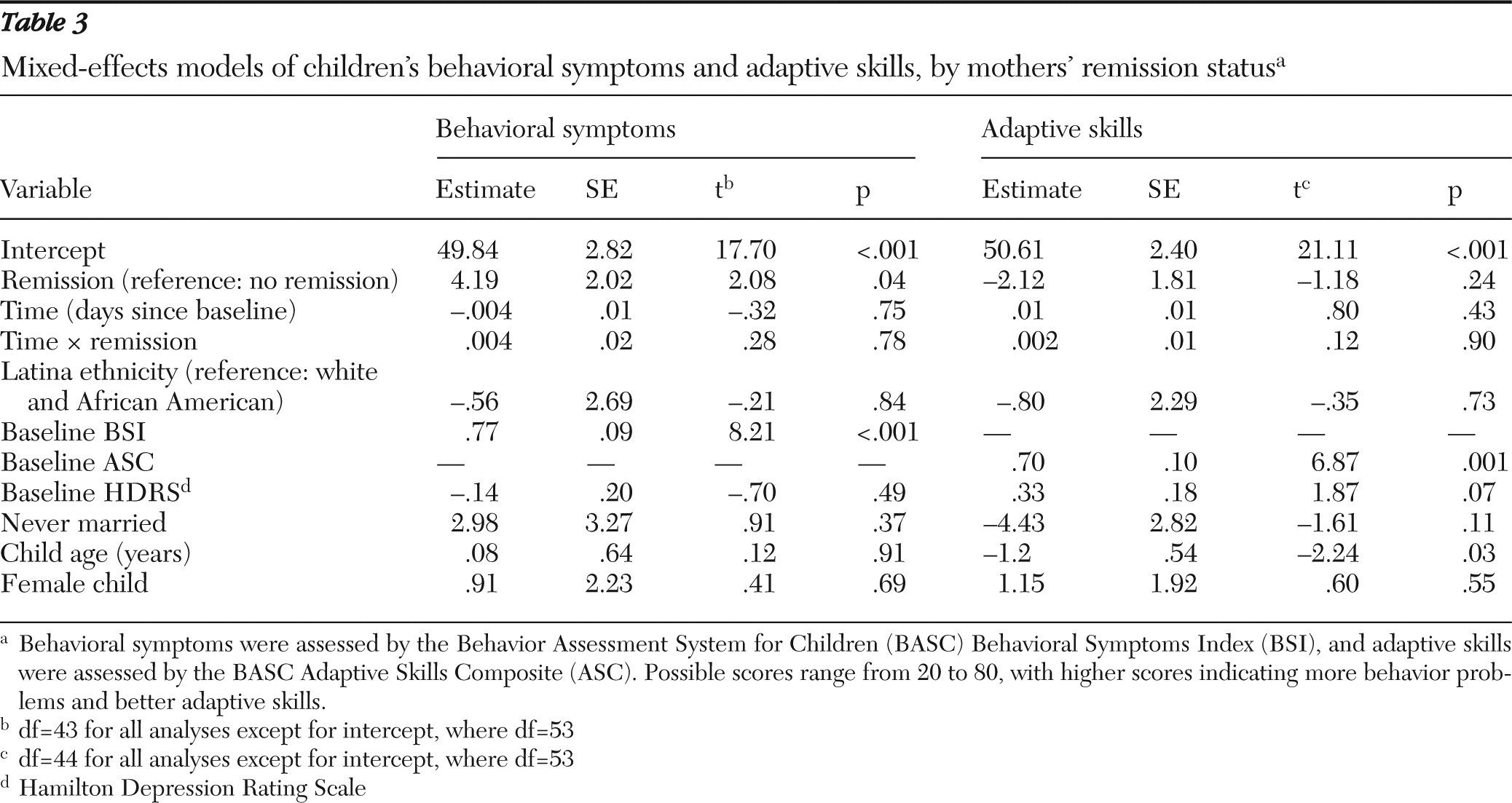
A total of 19 (32%) women were classified as in remission for depression at six months, and 17 (28%) women were classified as achieving remission at 12 months.
Models with both random intercept and random slope effects failed to converge because the variance for the slope was close to zero, so random intercept-only models were used. The overall multivariate F test for this model indicated that among children with similar levels of behavior problems at baseline, those whose mothers' depression remitted had significantly fewer behavior problems than children of mothers whose depression had not remitted, at both six- and 12-month follow-ups, with an overall difference of 4.2 on the BSI (t=2.08, df=43, p=.04). The remission × time interaction term was not significant, indicating that this difference between the remission groups did not vary over time (
Table 3).
Similar analyses were conducted to examine children's adaptive skills as a function of whether mothers' depression had remitted at the six- and 12-month follow-ups. Random intercept-only models were again used. The overall multivariate F test indicated that among children with similar baseline levels of adaptive skills, there were no significant differences in adaptive skills according to mothers' remission status at either time point, nor was the interaction term for remission status × time significant.
Discussion
The goal of this study was to examine whether treating mothers' depression could reduce or eliminate the substantial negative effects of maternal depression on children's behavior problems and adaptive skills. The study extended previous literature by evaluating outcomes of children as a function of their mothers' depression treatment within a randomized controlled design, evaluating the effect of remission prospectively and for one year, and comparing children of parents treated with medication and psychotherapy.
Random assignment to active treatment for depression, either medication or psychotherapy, successfully reduced mothers' depression symptoms but did not result in improved child outcomes. Although Miranda and colleagues (
17) reported that women in the larger sample were more compliant with, and achieved a stronger response from, medication versus CBT, our study provided no evidence that this benefit extended to their children. Children of mothers whose depression remitted, whether this occurred spontaneously or was associated with treatment, had fewer behavior problems at both the six- and 12-month follow-ups than children whose mothers remained depressed, even after analyses controlled for baseline differences between the two groups in maternal depression levels and child behavior. Such improvement was not observed for adaptive skills. These findings were generally consistent with the conclusions of Pilowsky and others (
10) and Garber and others (
11), who reported that remission of parental depression was associated with decreases in child psychiatric symptoms and diagnoses.
Our ability to conduct both experimental (intent-to-treat) and nonexperimental analyses allowed us to draw several conclusions. First, the failure to find effects for random assignment to treatment means that we cannot conclude that treating maternal depression causes improvement in child well-being. The finding that remission was associated with improvement in children's behavior problems is not acceptable evidence of causality, as third variables may actually explain which mothers and children improve. Second, on the basis of these results, we cannot conclude that screening low-income women for depression in primary care settings or expanding access to mental health services among depressed mothers, particularly those not initially seeking treatment, will benefit children.
There are several possible reasons for these findings. First, relatively few women received an adequate course of treatment despite intense efforts to engage and maintain them in treatment. Even among those who improved, not all experienced a full and consistent remission over the one-year period, consistent with other clinical trials examining low-income, single mothers (
8). The improvement of mothers whose depression was successfully treated was not sufficient to create significant effects for the entire group of children in the intent-to-treat analysis. Partial remission of maternal symptoms may not produce improvements in the parenting and family environments that likely mediate effects of depression on children (
2,
10,
19).
However, the positive association between maternal remission and children's behavior problems indicates that when women's symptoms do improve, their children experience some benefit, regardless of the reason for the remission. The reduction by approximately 4 points, or almost one-half of a standard deviation, on the BSI is meaningful and did not attenuate from the six-month to 12-month follow-up. Consequently, these results suggest that modest improvements in children's behavior occur when their mothers' depression remits.
These findings should be considered in light of some study limitations. Low rates of exposure to full treatment likely attenuated the potential effects of treatment on children, although, again, the efforts to maintain women in active treatment were substantially more intensive and persistent than are possible in routine depression care. In addition, although these children of depressed mothers had more behavior problems than children of nondepressed mothers (
14), because their initial mean BASC scores were not in the clinical range they evidenced lower rates of psychopathology than typically reported in samples recruited through mental health settings (
10). We did not examine factors that may moderate treatment effectiveness, such as severity of maternal depression, presence of comorbid disorders (
20–
22), or presence of fathers in the home (
8). Also unknown is the extent to which these results generalize to children of different ages and from families that are not from minority racial-ethnic groups.
Finally, all data were based on mothers' reports. Depression is known to cause a small but significant negative bias in ratings (
23,
24), an effect also observed for this sample of mothers, whose baseline ratings of their children indicated more behavior problems compared with the ratings of fathers and teachers (
14). We were not able to examine fathers' and teachers' ratings at the six- and 12-month follow-ups, because low participation rates and changes in father figures and teachers made it impossible to impute missing data.
Conclusions
Among these low-income mothers with major depression, primarily from minority groups, access to evidence-based treatment for depression was insufficient to ensure that their four- to 11-year-old children would experience relief from the effects of the depression. However, the association between remission of maternal depression and improvement in mother-reported children's outcomes, consistent with prior research (
8,
9), suggests the importance of increasing remission rates among depressed mothers.
Certainly, expanding access to care and offering additional evidence-based treatment to nonresponders are necessary but not sufficient first steps. Educating depressed parents and other family members about both depression treatments and the effects of depression on children (
25) and adapting treatments to address the barriers faced by low-income, often single, mothers may also be critical (
26–
28). Furthermore, these results argue for the importance of pursuing more innovative approaches to preventing mental health problems among offspring of depressed parents.
Recent randomized trials seeking to prevent psychopathology among offspring of depressed parents suggest promising approaches. These include Garber and others' (
29) group cognitive-behavioral program for adolescents, Compas and others' (
30) family-based prevention program, which targeted both youth coping skills and parenting skills, and Riley and others' (
31) and Valdez and others' (
32) pilot family-based prevention program at outpatient mental health clinics. Such two-generation programs, while promising, are costly, pointing to the need for a systematic examination of whether the most effective approach to treating and preventing mental health problems among the offspring of depressed parents is to target the depressed parent, the offspring, or both (
33).
Further research is also needed to examine the extent to which parental depression severity and chronicity moderate the effects of prevention efforts as well as factors that mediate the effects of prevention efforts, such as cognitive restructuring, improved coping skills, and better parenting (
2,
11,
29–
33). Finally, research is needed on the long-term effects on families of treating mothers' depressive episodes to determine whether the benefits of remission persist.
Acknowledgments and disclosures
This research was supported by grants MH58384 and MH56864 from the National Institute of Mental Health. The authors gratefully acknowledge data analytic support from Lily Zhang, M.S. This work was conducted before Dr. Broitman began official duties as a U.S. government employee.
The authors report no competing interests.