Telemental health services have revolutionized mental health care delivery in the U.S. Department of Veterans Affairs (VA) by expanding access to mental health services through the use of remote videoconferencing. The VA has taken a leadership role in telemental health innovation since the 1960s, when it used telemental health videoconferencing to connect the VA facilities in Omaha, Lincoln, and Grand Island, Nebraska, with the University of Nebraska (
1). Later, in 1970, telemental health videoconferencing was used to connect the VA facility in Bedford, Massachusetts, to Massachusetts General Hospital (
2).
With the expansion of telehealth technologies in the past decade, the VA undertook a major initiative to develop existing telemental health services into a nationwide telemental health clinical and technical infrastructure. As a result, from 2003 to 2011, telemental health services in the VA have increased steadily more than tenfold; since 2003 the VA has documented nearly 500,000 telemental health encounters (
3).
Feasibility and small-scale randomized controlled studies have demonstrated the equivalence of telemental and face-to-face treatment (
4,
5), but no national studies to date have reported outcomes of telemental health services among large populations. This article reports a national study of clinical outcomes of nearly 100,000 new telemental health patients treated by the VA from 2006 to 2010. The study specifically addressed rates of inpatient psychiatric hospitalization among the patients before and after their entry into telemental health services. Its hypothesis was that patients with increased access to mental health services through remote technologies would demonstrate decreased hospital utilization, as evidenced by decreased number of admissions and days of hospitalization.
Methods
The study used a performance-improvement dashboard created by the VA to assess nationwide clinical outcomes of telemental health patients. The dashboard used aggregate VA administrative data that had been stripped of individual patient information or identifiers. Data were obtained for all patients who received mental health services by remote high-speed videoconferencing for the first time between 2006 and 2010. Telemental health encounters were defined by a primary VA mental health visit code and a secondary telehealth code. Newly enrolled telemental health patients did not have any visits coded as telehealth in the prior 12 months.
The performance-improvement dashboard provided aggregate national data comparing patients' acute psychiatric inpatient utilization during each fiscal year (FY) before and after the patients' enrollment in telemental health services (
3). A FY is the 12-month period from October 1 to September 30. Utilization was quantified as the number of hospital admissions and the total number of days hospitalized in inpatient treatment on acute general psychiatry, substance abuse, and posttraumatic stress disorder units. Long-term psychiatric hospitalization placements and residential treatment were excluded from these data.
All patients within the national VA health care system who were new to telemental health care during this period were included in this analysis, regardless of whether they had inpatient activity during that period. To establish a comparison period before use of telemental health services, the study determined the total amount of time of telemental health activity for each new patient in each FY and then retrieved retrospective data for the equivalent amount of time from the first date of telemental health activity up to 12 months.
This study focused on clinic-based, high-speed videoconferencing and did not include any home telehealth encounters. Mental health patients were referred for telecare by clinicians. Typically, telemental health services were provided remotely at community-based outpatient clinics by mental health providers of all disciplines located at larger parent VA hospital facilities. Equipment consisted of either room or personal desktop videoconferencing units transmitting at 384 kbps or greater.
The study included telemental health services for all psychiatric diagnoses and all clinical types of telemental health visits by videoconferencing, including intakes, urgent care visits, medication management, individual therapy, group therapy, and family therapy. The study was reviewed and approved by the VA Connecticut Healthcare System Institutional Review Board.
Results
From October 1, 2006, through September 30, 2010, a total of 98,609 patients were newly enrolled in VA telemental health services throughout the United States. Consistent with the VA's patient demographic characteristics, men (N=90,175) constituted 91% and women (N=8,434) constituted 9% of the sample. By age, 2.3% were 25 or younger, 9.5% were 25–34, 10.6% were 35–44, 18.6% were 45–54, 40.8% were 55–64, 10.3% were 65–74, 6.1% were 75–84, 1.7% were 84–94, and less than 1% were 95 or older. Patients were enrolled in telemental health services for an average of 182 days.
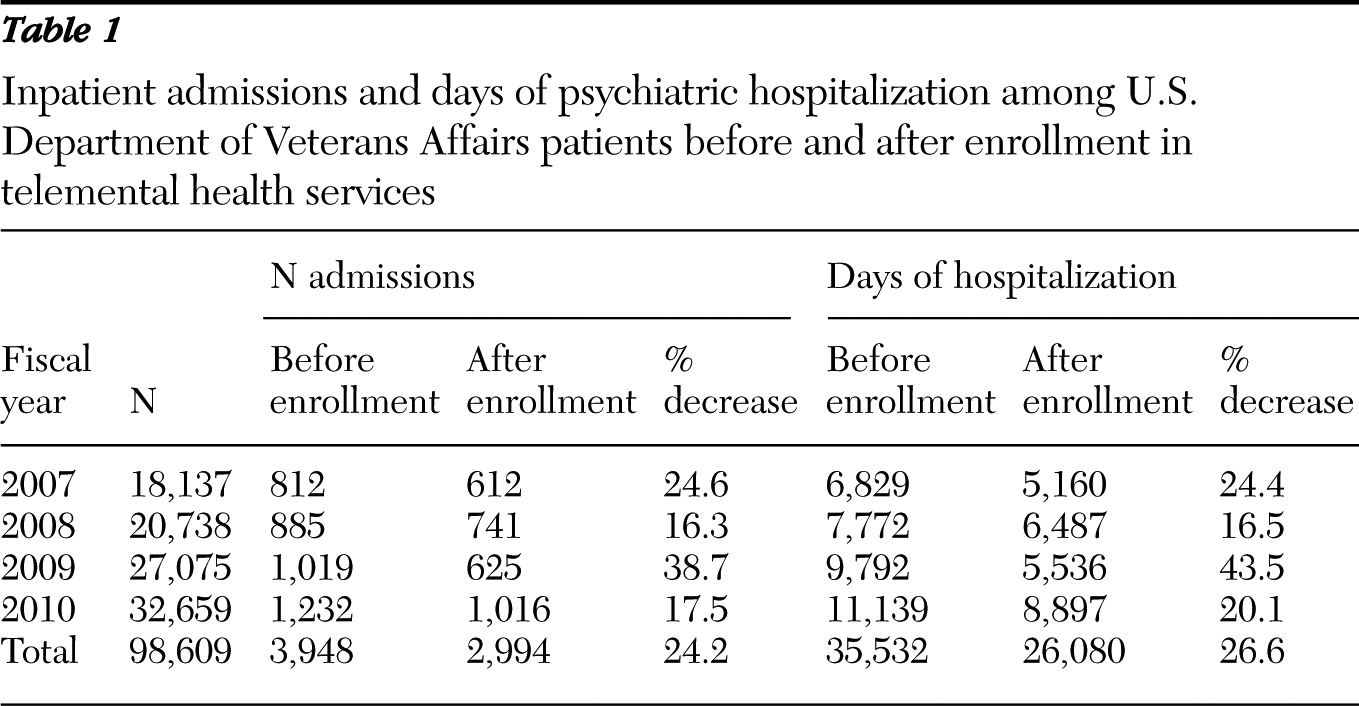
National hospitalization outcomes data, expressed in number of admissions and days of psychiatric hospitalization, for the sample are presented in
Table 1. The total number of admissions among telemental health patients dropped from 3,948 before enrollment to 2,994 after enrollment, a decrease in cumulative average for the four FYs of 24.2%. The total days of hospitalization fell from 35,532 before enrollment to 26,080 after enrollment, a decrease in cumulative average for the four FYs of 26.6%. The total number of admissions and days of acute hospitalization declined after enrollment in telemental health services during all four years.
Decreases in hospitalization days and admissions were consistent across male and female subgroups for all years. Decreases in days of hospitalization and admissions were demonstrated by 83.3% of all age groups across all years, with the exception of occasional increases among the patients who were younger than 25 to 34 years old and among the patients age 65 to 84.
Discussion
This report is the first to describe outcomes of telemental health patients on a large scale. Small-scale studies have focused on feasibility and on randomized control design (
4–
6). National reports about telehealth services have been limited to description, to smaller subsets of the population, or to measures not specific to mental health populations (
7–
9).
The VA is uniquely positioned to provide information about outcomes of telemental health for a large population because of the size of its national telemental health network and because it has the data capabilities from electronic medical records necessary to capture, collect, and analyze outcomes information. Although the VA has already reported on home-based, telemental health programs (
10–
12), this study is the first to assess outcomes of large-scale telemental health services that used clinic-based videoconferencing.
This study provided initial data demonstrating that patients enrolled in telemental health services experienced decreased numbers of admissions and days of psychiatric hospitalization. The decreased hospitalization utilization rates for mental health patients may be explained by increased access to services through remote care delivery. These services include evidence-based psychotherapy, patient-education groups, and closer management of medications leading to increased treatment adherence. Furthermore, remote clinical videoconferencing may circumvent the need for hospitalization by affording mental health clinicians with opportunities to provide immediate intervention for patients on the verge of decompensation or dangerousness (
13).
Although we cannot rule out explanations for decreased hospitalization rates that are unrelated to the telemental health intervention, the overall VA population of mental health patients did not demonstrate similar decreases during this period. Instead VA patients receiving mental health services experienced a slight increase in number of episodes of inpatient care and little change in number of days of hospitalization in contrast to the telemental health cohort (
14).
Because this study was limited in its degree of analysis, further evaluation will examine more specific subpopulations of patients, such as those with different diagnoses or who live in different geographic areas; will focus on the subgroup of hospitalized patients; will examine hospitalization rates for a period exceeding six months; and will add cost analysis components comparable to those used by the smaller-scale evaluations in the literature (
15). The increase in rates of admissions and days hospitalized occasionally experienced by patients in specific age groups warrants more detailed evaluation to determine whether particular age groups experienced unique challenges that prompted greater hospitalization, such as the onset of illness among younger patients or the predominance of specific diagnoses in other age groups.
Finally, given that this study lacked a specific control group, future work will provide more elaborate comparisons of outcomes among telemental health patients and matched face-to-face patients. Such studies can determine whether patients receiving telemental health services experience decreased hospitalization utilization compared with patients in standard care and whether telemental health care may be superior to standard care in particular circumstances.
Conclusions
This study of 98,609 patients is the first to report outcomes of telemental health services in a large population. It demonstrated that hospitalization utilization during FYs 2006–2010 decreased by an average of approximately one-fourth after initiation of telemental health services. The results support the expansion and further evaluation of telemental health services.
Acknowledgments and disclosures
The authors report no competing interests.