Continuity of care between inpatient and outpatient psychiatric settings, including the communication of key treatment information and linkage of the patient to an outpatient clinic and service staff, is essential for maximizing outcomes such as recovery and quality of life among persons with a severe mental illness (
1). Continuity between treatment settings can be defined as an uninterrupted flow of services and clinical information during transition from inpatient to outpatient care. The relationship between seamless care transition and rehospitalization is of great interest because of the personal costs, such as derailment of recovery and disturbance in relationships, and the economic costs of readmission. In fact, hospitalization is the most expensive health component in the treatment of individuals with a severe mental illness (
2).
Research indicates that the strongest predictors of psychiatric readmission include poor therapeutic alliances, nonadherence to medication and outpatient appointments, and a history of psychiatric hospitalizations (
3–
5). It has been estimated that among patients with a severe mental illness, 30% to 40% are rehospitalized within six months of discharge, 35% to 50% are rehospitalized after one year, and 65% to 75% are rehospitalized within five years (
6–
8). The costs associated with such relapses are up to five times higher than the costs of treatment for patients who are not readmitted (
9). Substantial evidence indicates that patients who are not engaged in postdischarge care, including medication appointments, experience significantly higher recidivism rates than patients who participate in aftercare treatment (
10,
11).
Even minimal contact with aftercare treatment is associated with lower recidivism rates (
11,
12); conversely, delays seeking outpatient care after psychiatric hospitalization are linked to poorer outcomes (
10,
13). These studies indicate that the months immediately postdischarge appear critically important for implementing strategies to improve engagement in outpatient treatment.
Despite these data, a review article by Kreyenbuhl and colleagues (
14) revealed that a median of 58% of patients fail to engage in postdischarge outpatient treatment (range 18%–67%) (
14). The most consistent predictors of successful transition to outpatient care are the use of bridging strategies by the treatment team (
15,
16). These linking strategies involve coordination of ongoing treatment between inpatient and outpatient staff, communication regarding past and present use of specific medications, and consideration of psychosocial factors (
17).
Studies examining the effect of interventions to increase aftercare engagement and decrease rehospitalization show mixed results, depending on the outcome variable. Dixon and colleagues (
15) reported that a brief intervention implemented after discharge increased engagement, although no effect on rehospitalization was found. In an older sample of 59 psychiatric inpatients, Kopelowicz and others (
16) found that patients with schizophrenia who participated in a reentry program for one month postdischarge were significantly more likely to attend their first aftercare appointment. Although one study associated day treatment with a significant reduction in future admissions (
12), a review article of four randomized trials concluded that there was insufficient evidence to deem such intense treatment effective (
18).
Continuity of care is considered an important component of high-quality care for persons with a severe mental illness, but there is little recent research on postdischarge interventions. Implementation of these linking practices in community mental health settings has been slow and erratic, possibly because of inadequate funding but also because savings from reduced hospitalization do not accrue to the outpatient provider.
Filling a gap in current research, this article describes a demonstration program assessing effectiveness of a continuity-of-care intervention, the medication management coordinator program, in which a psychiatric nurse or medical case manager makes contact with patients during psychiatric hospitalization and works with them continually for six months posthospitalization. We hypothesized that patients who received medication management services would experience better aftercare engagement and fewer hospitalizations and utilize fewer crisis or emergency services throughout the treatment period compared with patients who did not participate in the intervention.
This study analyzed existing data and was conducted after the conclusion of the project. Therefore, it was deemed exempt by the Institutional Review Board of the University of Texas Health Science Center at San Antonio. Because the program was implemented as an add-on to normal clinic procedures, no consent form was utilized.
Methods
Setting and design
The study was conducted at two Center for Health Care Services (CHCS) clinics in Bexar County, Texas, a locality that is home to 1.7 million residents and includes San Antonio. Nonrandomized enrollment of 670 hospitalized patients occurred between October 2005 and August 2007 as a demonstration project at a community mental health agency. All persons identified as meeting criteria were enrolled in the program and evaluated on an intent-to-treat basis.
The medication management coordinator program was implemented at one clinic. Patients at the other clinic who met eligibility criteria served as comparison subjects over the same follow-up period. The clinics shared management and were ten miles apart. Medication management coordinators were hired for the sole purpose of this project and, as such, did not typically assume other case management or nursing duties performed by routine clinic staff. The program had a separate funding source, and services delivered by the coordinators were not billed by the clinic.
Participants
Eligible program participants had diagnoses of schizophrenia or schizoaffective or bipolar disorder; were hospitalized for a mental illness; and had outpatient follow-up at one of the two clinics. The addition of bipolar disorder as an inclusion criterion in year 2 because of lower-than-expected enrollment numbers resulted in relatively more participants with disorders on the schizophrenia spectrum at program's end. Patients in assertive community treatment (ACT) programs were not eligible. Inpatient logs at two private and one state hospital were reviewed daily to identify eligible participants, and most participants (N=207) were recruited during their hospitalization. However, approximately one-third were recruited within 30 days of discharge at their initial CHCS clinic appointment (N=118).
Intervention description
The medication management coordinator program was implemented under the supervision of the demonstration program psychiatrist. Medication management personnel included registered nurses and bachelor's-level case managers given intensive training about severe mental illness and psychopharmacology. Medication management coordinators were clinically supervised by a psychiatrist and a Doctor of Pharmacy throughout the project. For patients recruited at the psychiatric hospitals, the coordinators established a relationship before discharge. As part of this process, the coordinator obtained a clinical history, including previous locations of treatment. If the participants had been patients of the CHCS in the past, the coordinator reviewed their outpatient charts to develop a thorough summary of previous medications, treatment outcomes, and appointment keeping and used physician progress notes to estimate medication adherence.
Before a patient's discharge, the coordinator reviewed the date and time of the outpatient appointment with the participant and offered an appointment card and map to the clinic. Possible impediments to attending the appointment, such as transportation difficulties, and solutions to such problems were discussed. After discharge, the coordinator met with the participant at each outpatient visit to assess clinical status, medications, and side effects, compliance issues, and other problems and to provide medication education.
Information from each visit with a medication management coordinator was given to the treating psychiatrist prior to an appointment with the participant. The psychiatrist was also given medication recommendations from the Texas Implementation of Medication Algorithms (TIMA) guidelines. These guidelines include medication algorithms for schizophrenia (
19) and bipolar disorder (
20), brief scales to monitor symptoms and side effects, and a psychoeducational program for patients and families (
21,
22). Manuals detailing TIMA guidelines were developed in collaboration with the Texas Department of State Health Services and were available during this project through that agency's Web site (
www.dshs.state.tx.us/mhprograms).
Medication management coordinators continued to see participants during the six-month program period. Program goals were to enhance participant engagement in care, improve continuity of medication management during transition from inpatient to outpatient care, improve information available to the treating psychiatrists, improve TIMA-guideline implementation, and reduce hospital and crisis admissions.
Data sources and measures
Data were gathered for the 12-month period before participants' enrollment in the medication management program (baseline), during the six months of the medication management intervention, and for six months after the intervention ended (follow-up).
Independent assessors, not involved in program implementation, collected service utilization data about the patients who participated in the intervention and the patients who served as the comparison group. Data were obtained from local hospitals (state, private nonprofit, and county), CHCS records, and Medicaid files. The main outcomes were the number of medication appointments, nurse or case manager contact hours (including contact with medication management coordinators or routine contact with clinic staff), number of admissions and hospital days, time (days) to rehospitalization, and number of crisis or emergency visits. Patients were characterized as moderate-high utilizers (two or more medication visits) or minimal utilizers (zero or one medication visit) at baseline, during the intervention, and at follow-up. Covariates included intervention status, age, race, sex, education, income, living situation—such as supervised board and care or living with family or on one's own—and Medicaid status.
Data analysis
Descriptive analyses included calculation of means with standard deviations and frequencies for all variables; chi square analyses assessed bivariate associations. Outcomes were analyzed by using repeated-measures analysis of covariance that adjusted for baseline (preintervention) scores. The independent effects of the medication management coordination program on postdischarge health care utilization were determined by using a Poisson or negative binomial regression for count data and a logistic regression for dichotomous data. Utilization data were annualized to account for differences in the length of time of the three time periods.
To avoid bias toward the intervention program, we excluded from analyses involving appointment keeping the 118 persons enrolled at the time of their first outpatient medication appointment. Time (days) to first follow-up medication appointment and days to rehospitalization were analyzed by using Cox proportional hazards models.
Results
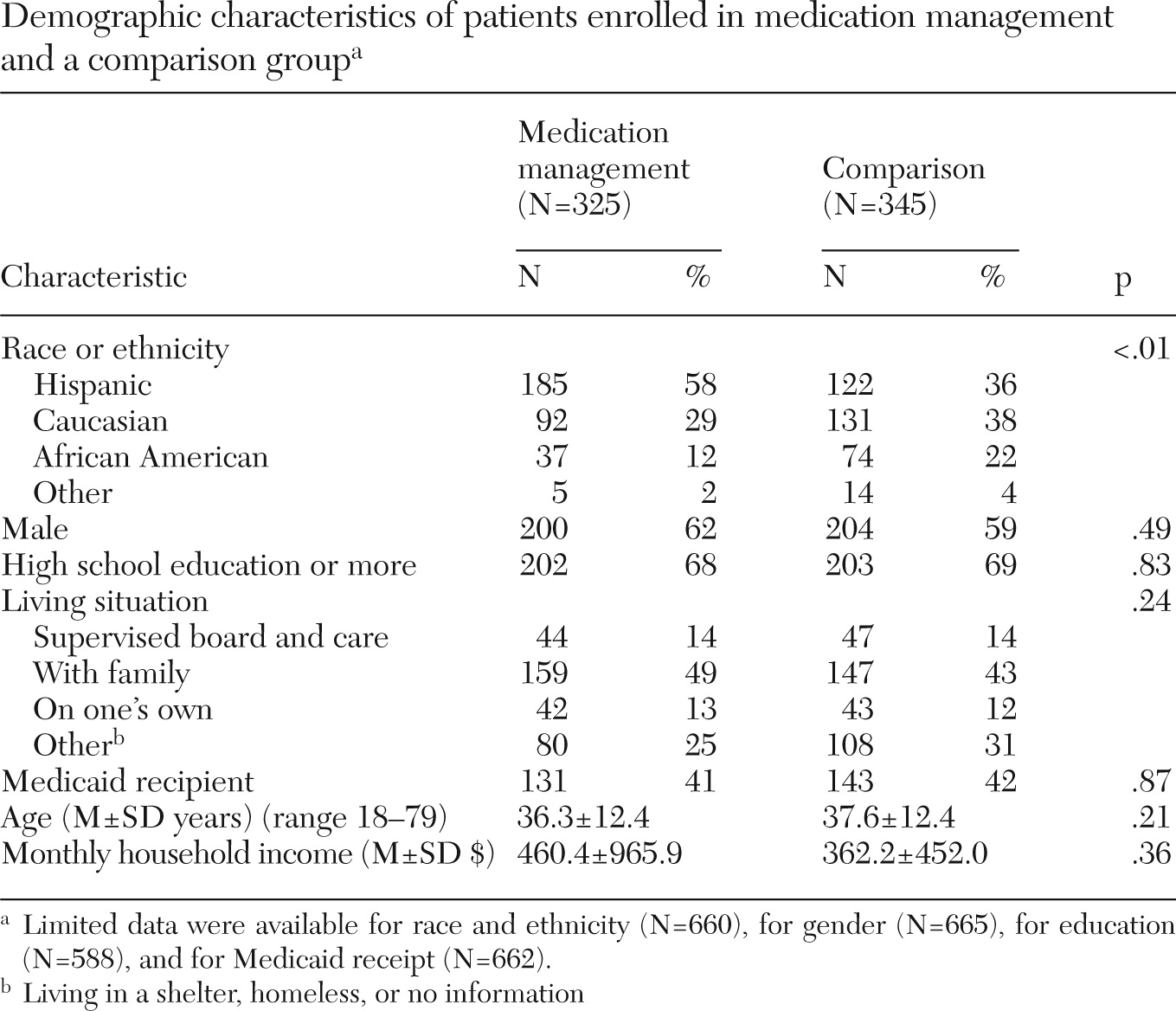
Of 670 participants, 325 (49%) were enrolled in the medication management coordination program, and 345 (51%) were the comparison group. Demographic variables are summarized in
Table 1. The only significant difference between the two groups of participants was that participants in the medication management program were more likely to be Hispanic (
χ2=35.7, df=3, p<.01). This difference reflected the demographic characteristics of the catchment areas of the clinics.
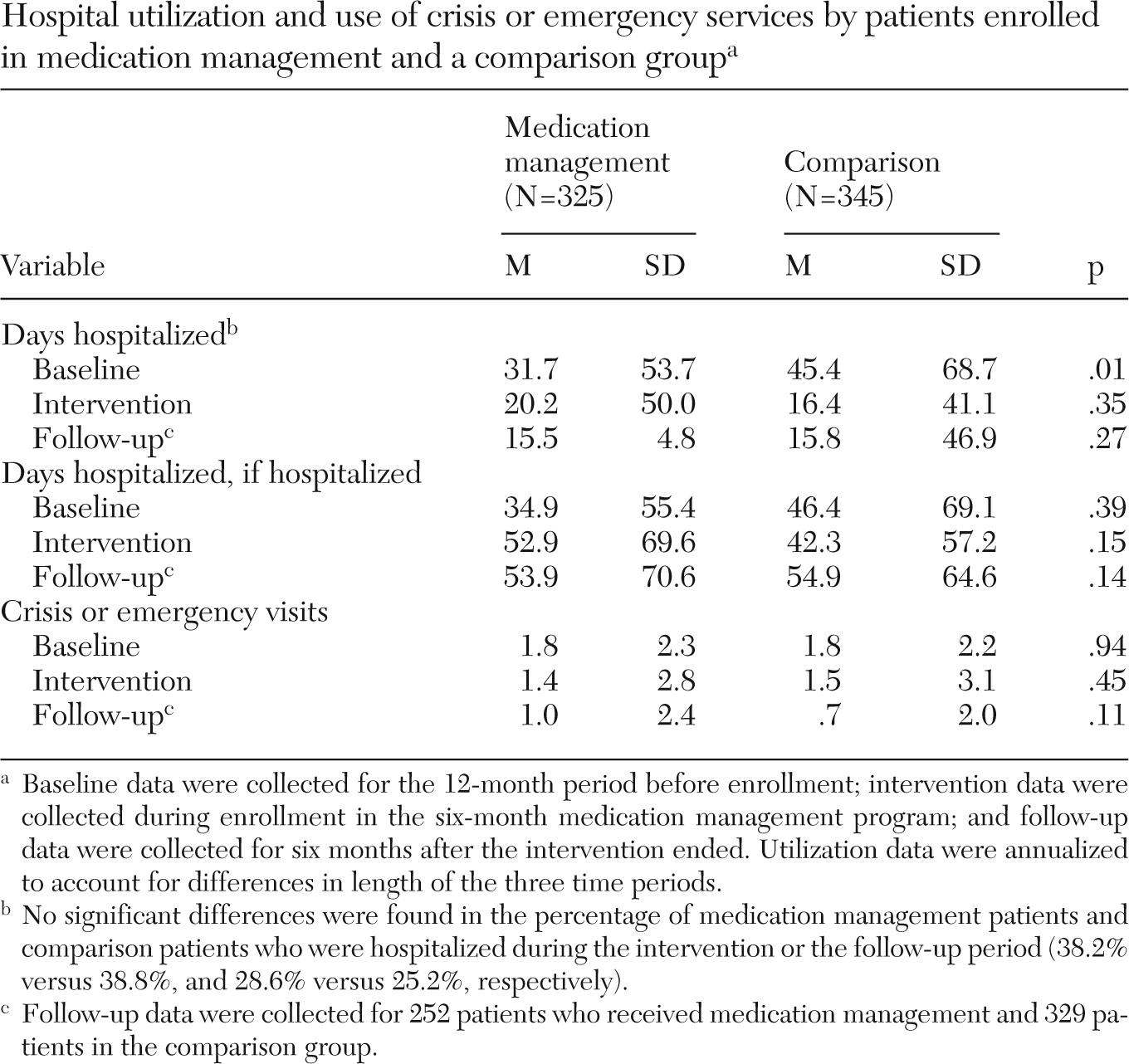
Bivariate analysis indicated that at baseline, patients in the comparison group had spent an average of 13 more days in the hospital than patients in the medication management program (
Table 2). Use of both inpatient and crisis or emergency services by both groups declined over the study period (results not shown). Because of these findings, preintervention utilization was used as an additional model covariate. The multivariable generalized estimating equation model showed that consistent with the unadjusted, bivariate results, utilization declined significantly over time even after adjusting for covariates (main effect of time). This decline was similar for both groups (p<.01), and there was no interaction effect of time by medication management group.
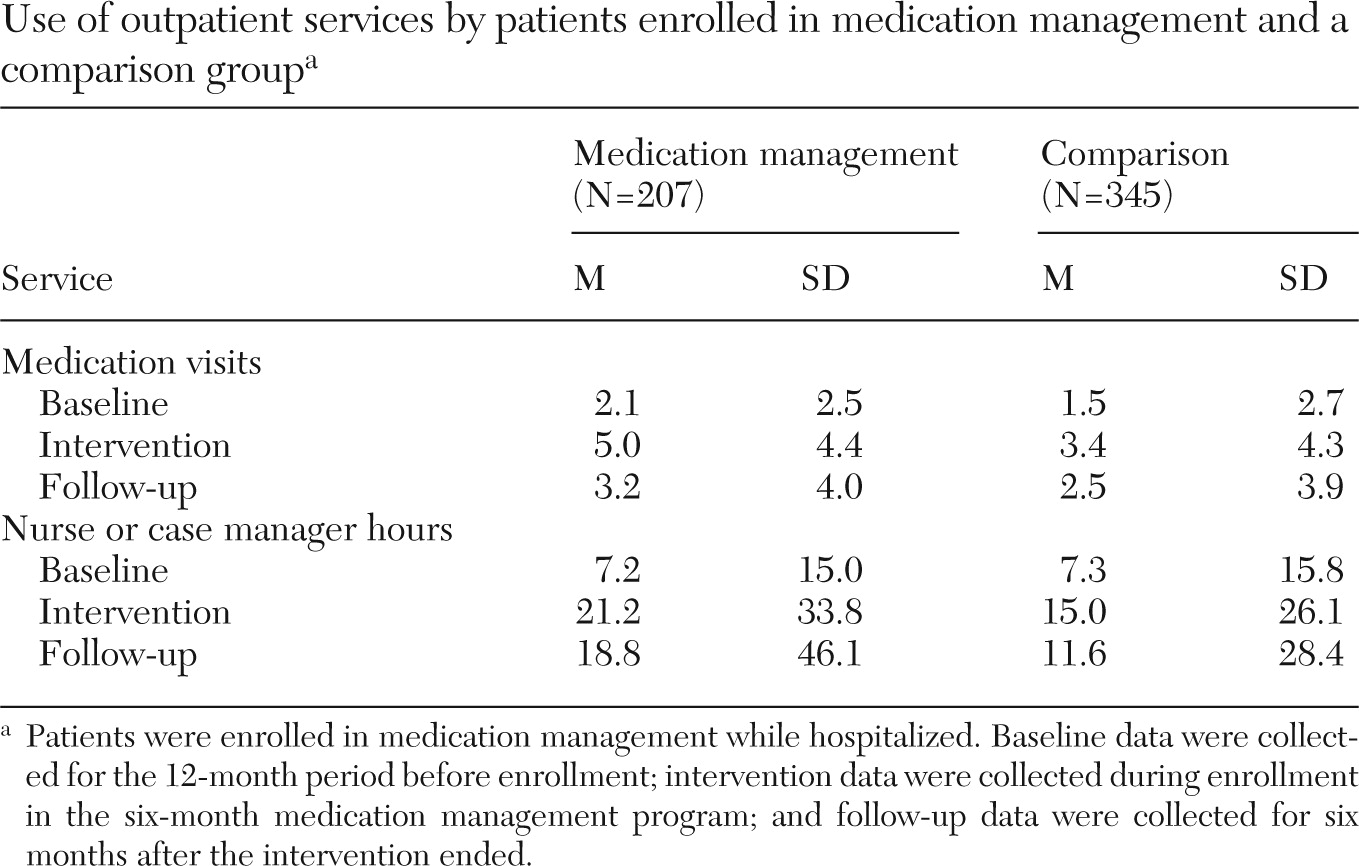
Participants in the medication management program attended more medication appointments than did comparison-group participants during the treatment (5.0 versus 3.4) and follow-up (3.2 versus 2.5) periods (
Table 3). After adjustment for baseline utilization, a significant interaction effect for group × time (
χ2=3.96, df=1, p<.05) and individual main effects for time (
χ2=101.23, df=1, p<.001) and group (
χ2=42.66, df=1, p<.001) were evident. Use of medication visits by both groups decreased over time but decreased more precipitously among medication management patients.
Among the 544 patients recruited before discharge from the hospital, significantly more medication management participants than comparison group participants attended at least one outpatient visit with a physician within 30 days of discharge (odds ratio=2.64; χ2=36.30, p<.001) (data not shown). In regard to the combined nurse and case manager provider hours, the mixed-model analysis yielded a main effect by group (F=4.03, df=1 and 551, p<.05) and time (F=6.24, df=1 and 471, p<.05). Participants in the medication management program received more contact hours. No significant group × time interaction was found.
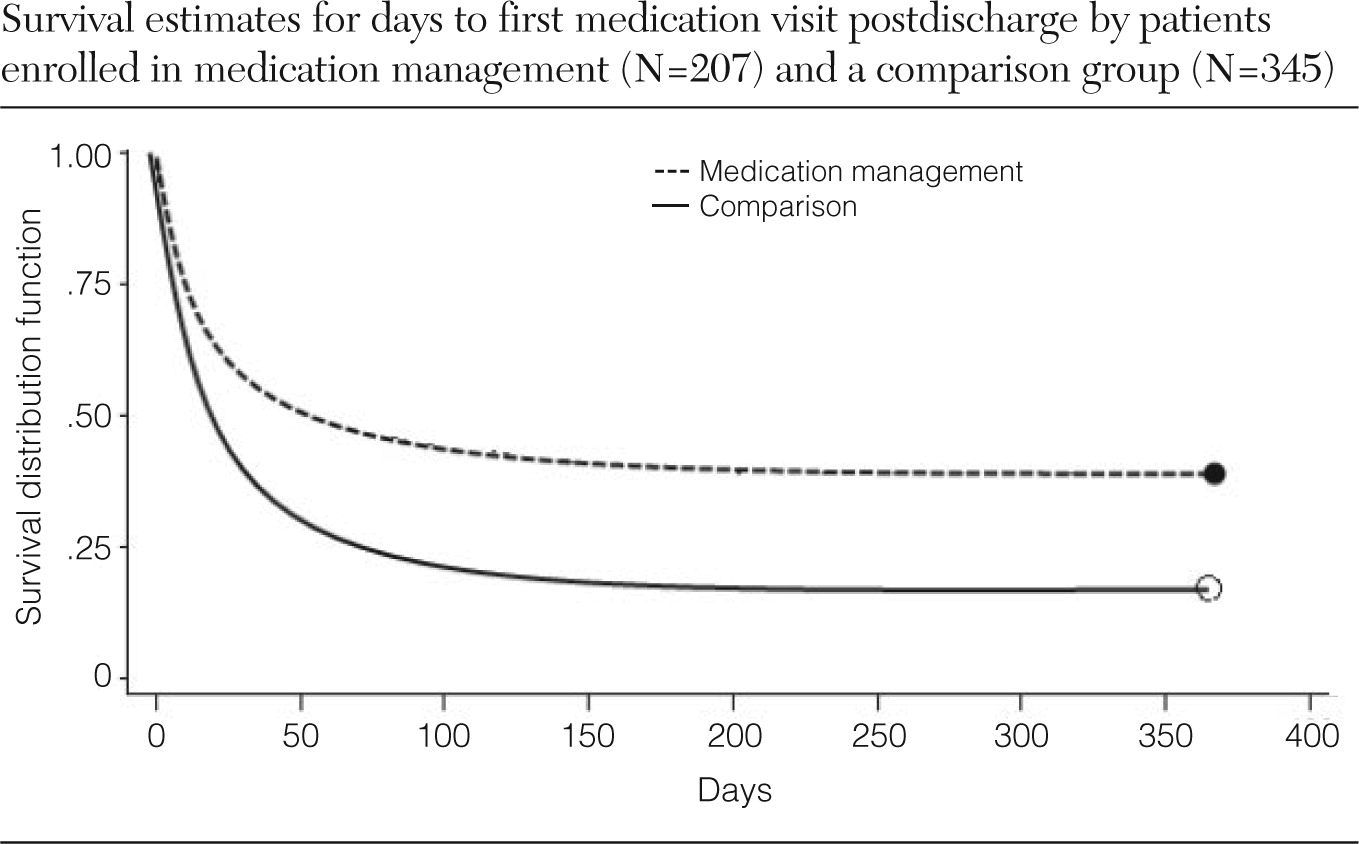
Participants in the medication management program took fewer days than comparison group participants to attend an outpatient medication appointment (84.34 versus 161.82 days; Kruskal-Wallis
χ2=26.87, df=1, p<.001). In the Cox proportional hazards model, time to first follow-up medication appointment differed by treatment group (
Figure 1). The median time to first medication visit was significantly less for the medication management group than for the comparison group (15 versus 60 days; log-rank test=32.09, df=1, p<.001). No difference was found between the groups on time to rehospitalization.
During each period, according to Medicaid and CHCS electronic data, many patients had no medication visits. Excluding the 118 individuals enrolled as outpatients, the data showed that 36 (17%) medication management participants and 135 (39%) comparison group participants—approximately one-third of all participants enrolled as inpatients—never attended a follow-up medication appointment (χ2=29.27, df=1, p<.001).
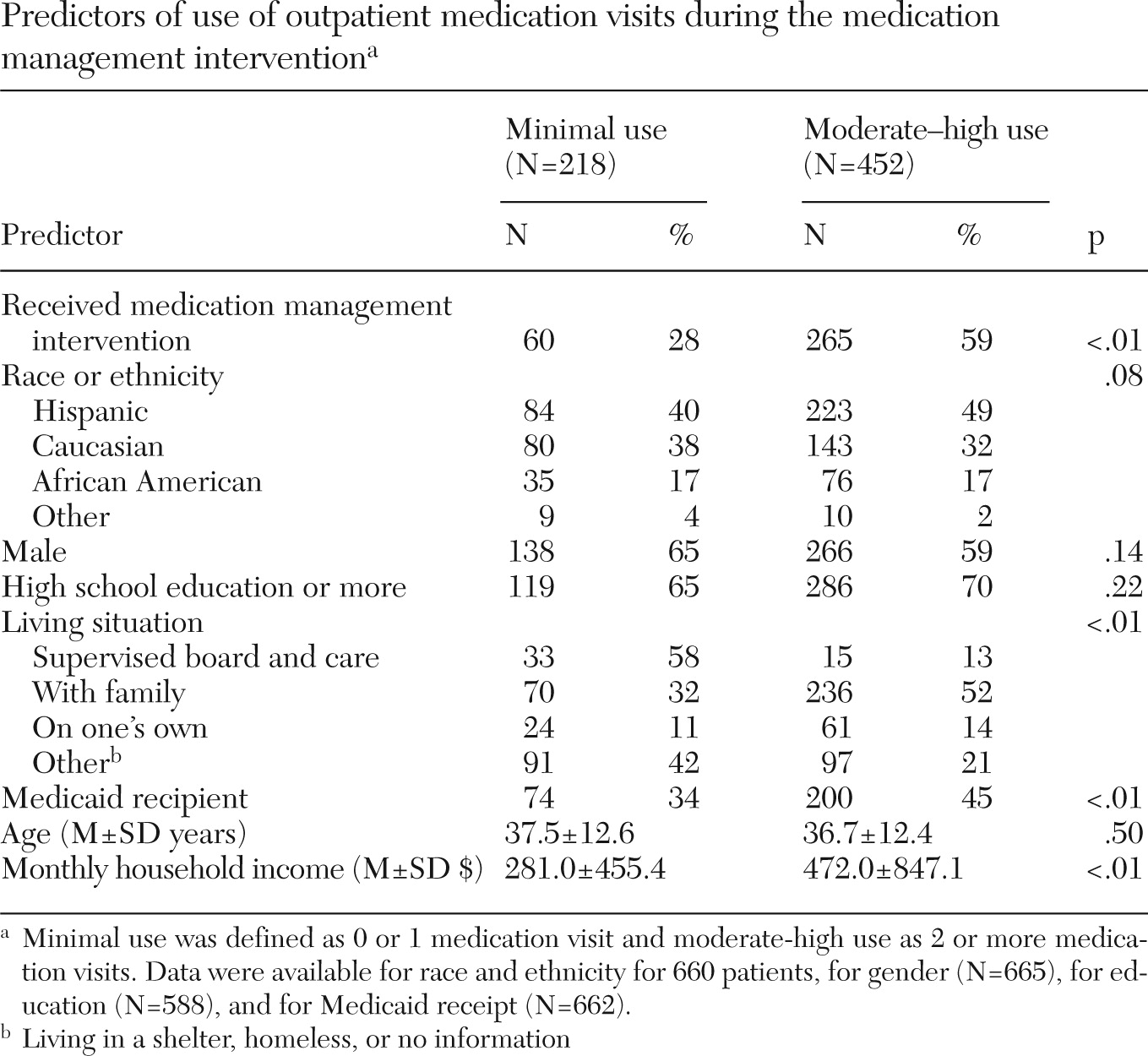
Persons living with family were more likely than persons living in other situations to have made two or more medication visits during the six-month intervention period (52% versus 32%;
χ2=35.9, df=3, p<.01) (
Table 4). Patients having two or more medication appointments had higher monthly incomes than patients with fewer medication visits ($472 versus $281; Kruskal-Wallis
χ2=24.20, df=1, p<.01). Medicaid recipients made up a higher percentage of the higher-utilization (45%) versus the lower-utilization (34%) group (
χ2=6.72, df=1, <.01). There were no significant effects of race, sex, educational attainment, or age.
Discussion
The results of this implementation project indicated that the medication management coordinator program succeeded in promoting earlier and more frequent engagement of patients with outpatient treatment after psychiatric hospitalization but did not have an impact on rates of rehospitalization or use of crisis or emergency services. Although the lack of an effect on use of high-cost services is disappointing from a fiscal perspective, it is an important finding in relation to efforts to redesign systems in cost-effective ways.
Improving patient engagement in postdischarge health care services is a necessary ingredient in reducing rehospitalizations. However, whether outpatient engagement, by itself, can sufficiently reduce acute exacerbations that require hospitalization is much less clear.
Reducing medication nonadherence, a major factor in symptom relapse in schizophrenia and bipolar disorder, represented a major aim of the intervention. In this demonstration project, we could not obtain independent measures of adherence, so the direct effects of the intervention on this parameter are unknown. Recent studies show the value of ongoing prompting of medication taking for adherence, and adding such prompts to this program might be helpful (
23,
24).
Social stressors, such as housing instability and substance abuse, are other contributors to relapse that were not directly targeted by the medication management intervention. The medication management coordinators made appropriate referrals when these problems were detected, but use of these referrals was not measured. Expansion of the medication management intervention to address these problem areas might further reduce rehospitalizations but would also add to the program's expense.
The finding that one-third of patients did not attend any medication visit postdischarge indicated significant difficulty with outpatient engagement of this population. Such engagement should be a priority among clinicians dealing with patients newly discharged from inpatient psychiatric care. The failure to engage in outpatient mental health care undermines efforts to sustain clinical improvements made during an inpatient stay. Our data indicated that improving engagement did not, per se, decrease rehospitalization, but poor engagement clearly impeded effective interventions. In our system, outpatient commitment is an option, but it is seldom used because of logistical and resource problems.
One limitation of this study was the lack of true randomization to medication management program status; instead, the study relied for comparison on a site not involved in the implementation. The separation of medication management and comparison patients by site avoided the problem of having two groups of patients within a single clinic. Because the project was confined to a single county, the results may not generalize to other regions with different levels of mental health resources and better integration of inpatient and outpatient care. Additionally, the program may have been enhanced by measuring the alliance between the medication management coordinator and the patient. A good working alliance takes time to develop and given the brief intervention period, it is possible that the lack of reduction in hospitalizations was attributable to this factor.
Finally, it is possible that selection of patients for programs aimed at increasing continuity between inpatient and outpatient care should be based on patient history. Olfson and colleagues (
7) reported that readmission risk increases most dramatically among patients with four or more previous hospitalizations. In addition, psychosocial treatments targeting the highest-risk patients have been found to significantly reduce psychiatric readmission (
10). On the other hand, patients with these characteristics often are best treated in ACT programs. Our goal was to test a much less intensive intervention for a population at significant risk for relapse and rehospitalization.
During the implementation of this demonstration project, several unexpected obstacles arose. First, medication management coordinators often found it difficult to obtain early notification from private hospitals regarding impending discharges, so that numerous individuals who were eligible for recruitment at the hospital were not recruited until they became outpatients. Additionally, because the total hospital stay in private facilities was usually fewer than seven days, it was difficult to gather all data from relevant sources to provide treatment histories to the inpatient physician for discharge planning. Shared or easily transferred electronic medical records would minimize the lack of information sharing by outpatient and inpatient prescribers about medication treatment. However, the differing goals of inpatient and outpatient physicians were related more to systemic issues, such as reimbursement structure, and they will not be overcome by improving the information flow between providers.
Finally, the medication management coordinator and the prescribing clinician could not always meet before a follow-up visit with the patient. Given that the prescribing clinicians were often overbooked, an inability to find time to discuss each patient was sometimes an obstacle in realizing program goals.
Conclusions
Our findings are consistent with prior studies documenting that disengagement among individuals with a severe mental illness from mental health treatment is correlated to symptom exacerbation, repeated hospitalizations, and homelessness (
14,
15,
25). Also in line with previous research, we found that patients with more family involvement and Medicaid coverage were more likely to attend postdischarge medication appointments. Although previous research has repeatedly found that younger age, male gender, minority racial and ethnic background, and lower educational attainment are linked with treatment disengagement (
12,
25), we found no such utilization differences. However, participants in this single-county sample were not demographically diverse, given that most were from minority racial and ethnic groups, had low incomes, and were relatively poorly educated.
In summary, in the post-deinstitutionalization era of mental health care, appropriate management of the transition from acute inpatient psychiatric treatment to outpatient status remains an understudied challenge. Observations from this study offer some hope that transitions may be improved through case management and medication education strategies and that ultimately, future readmissions can be reduced. Given the complex clinical and social needs of individuals with a severe mental illness, providing a smooth treatment trajectory is paramount in coordinating the multiple steps toward recovery and improved quality of life.
Acknowledgments and disclosures
This demonstration project was funded by AstraZeneca through a grant to the National Center for Behavioral Health Care Solutions, a 501(c)3 organization affiliated with the Center for Health Care Services. Additional support was provided by the U.S. Veterans Health Administration, the UT Health Science Center San Antonio, and Scott & White Healthcare. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the U.S. Department of Veterans Affairs or the U.S. government.
Dr. Zeber received a research grant in 2011–2012 from GlaxoSmithKline as principal investigator for one site of a multisite study unrelated to this article. Dr. Velligan is a consultant for or on the advisory boards of Ortho-McNeil Janssen Pharmaceuticals, Teva Pharmaceuticals, AstraZeneca Pharmaceuticals, Roche Genentech, Abbott Pharmaceuticals, Lilly Pharmaceuticals, Pfizer Pharmaceuticals, Bristol-Myers Squibb, Amgen, and Merck and Shire Pharmaceuticals. Dr. Miller is a member of the data monitoring committee for Otsuka and was on the advisory board of Myriad RBM in 2010. He has received investigator-initiated grant funding from Pfizer. The other authors report no competing interests.