Adjustment disorders encompass a diverse spectrum of disorders developed in response to a stressor. These diagnoses have been identified as prevalent within clinical samples, with an estimated 10% of primary care patients and 15% of inpatients meeting criteria (
1–
6) for these disorders. Despite this prevalence, the number of randomized trials and long-term follow-up studies for patients with adjustment disorders has been limited, although some studies have suggested that 30% of adults diagnosed with adjustment disorder develop another psychiatric disorder within 5 years of the initial diagnosis (
7). Treatment recommendations for adjustment disorders vary: investigations of pharmacologic and psychotherapeutic treatments have yielded mixed results (
8–
10). In the absence of clear treatment guidelines, the treatment and management received by patients for these disorders are widely heterogeneous, especially for patients with poor access to mental health services.
Given the clinical prevalence of adjustment disorder, it may be useful to describe how early treatment plays a role in the chronicity and severity of illness. We hypothesized that a descriptive study of the disorder derived from insurance claims data could provide a large population of cases encapsulating differences in treatment across geographic regions and providing longitudinal follow-up to yield insights into risk for severe outcomes. Because diagnosis of adjustment disorder is defined in close temporal proximity to a known stressor, the diagnosis may be subsequently revised or resolved. These diagnostic revisions may reflect manifestations of illness in relation to service utilization, which may clarify outcome expectations.
In this study, we used commercial claims data to examine the duration of adjustment disorder and rates of psychiatric diagnosis revision for patients after a new diagnosis of adjustment disorder. Subsequently, we used propensity score matching and inverse probability of treatment weighting (IPTW) to examine the effect of pharmacologic interventions, and benzodiazepines in particular, on rates of subsequent hospitalization for a psychiatric condition and overall.
Methods
This study was approved as nonhuman subjects research by the University of Chicago Institutional Review Board.
Data
Patients given a diagnosis of adjustment disorder were identified from the inpatient, outpatient, prescription drug, and other therapy claims files in the Truven Health MarketScan Commercial Claims and Encounters database (2003–2010), a claims database for privately insured patients in the United States. Patient-level covariates in this database include sex, age, decade of birth, insurance status, relationship to primary coverage holder, geographic census region, and an indicator of coverage for mental health services. Chronic disease index classifications and
ICD-9 organ system groups were assigned to patient diagnoses in accordance with Hwang et al. (
11) and the Healthcare Cost and Utilization Project of the Agency for Healthcare Research and Quality.
We collected county-level information on health care resources and demographic characteristics from the Health Resources and Services Administration’s 2010 Area Health Resources Files (AHRF). These files measure geographic variation in factors that may affect health status and health care in the United States. From the ARHF, we extracted the number of psychiatrists per 100,000 persons, median household income, and other data, including census population data, median age, education, race, and ethnicity variables.
Records with previous psychiatric diagnoses, psychotherapy, or psychoactive prescriptions prior to the diagnosis of adjustment disorder were excluded from the sample. Records with missing covariates or that could not be matched to a county were also excluded.
Statistical Analysis
We conducted a survival analysis for the complete sample of participants (N=200,760) to estimate the chronicity of adjustment disorder both to characterize the survival of the adjustment disorder diagnosis itself as a transient diagnosis and to characterize the diagnostic transition to other nontransient, psychiatric diagnoses. A nontransient psychiatric diagnosis was defined as any new psychiatric diagnosis classified as an ICD-9 mental disorder, including mood, psychotic, anxiety, and substance use disorders. ICD-9 diagnostic codes were chosen because of their uniformity in this data set in comparison with ICD-10 codes, which varied in availability across the period examined.
Hospitalizations, psychiatric and overall, were the outcomes of interest. IPTW was fitted by using a probit regression at the individual level with the inpatient, outpatient, and pharmacy claims observed at or prior to the initial date of diagnosis of an adjustment disorder (
12). Two treatments were primarily considered. Medication treatment was defined as having begun a psychotropic prescription within 1 month of a new adjustment disorder diagnosis. Psychotherapy treatment was defined as having begun psychotherapy within 1 month of a new adjustment disorder diagnosis. In addition, we conducted a subanalysis specifically for benzodiazepine treatment because of concern that poorer long-term outcomes, such as dementia, may be attributable to benzodiazepine use (
13,
14).
IPTW was based on individual-level covariates recorded at or before the observed date of diagnosis, in addition to county-level psychiatric services and demographic data with matched and unmatched means. Common support was defined by a 0.4 standard deviation caliper (
15). (A table that displays the IPTW matching pertaining to an analysis of a subgroup treated with benzodiazepine is available in the
online supplement to this article.) We fit a Cox proportional hazard model with the IPTW. All analyses were performed in Stata, version 15.1.
Results
The total sample contained 200,760 records of individual patients diagnosed as having adjustment disorder over a total of 2,772,881 months at risk. Of this sample, a significant number of records were excluded from the weighted analyses either because of missing data or because adequate covariate matches could not be identified across both treatment and control groups. The weighted analysis for the medication treatment group contained 26,645 individual cases over a total of 890,581 months at risk for psychiatric admission. The weighted analysis for the psychotherapy treatment group contained 33,562 cases over a total of 954,117 months at risk for psychiatric admission.
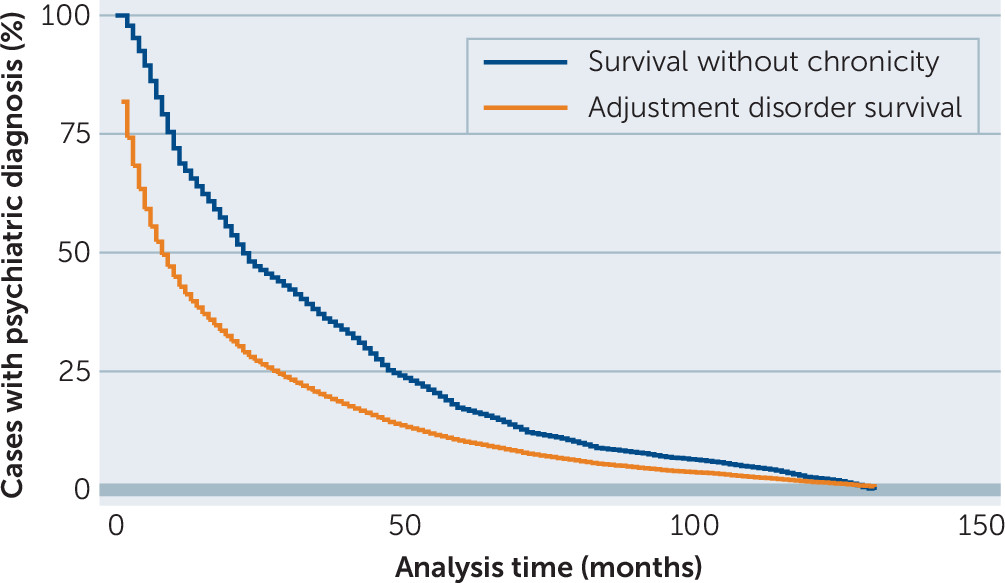
Duration of adjustment disorder diagnosis was estimated from the full sample of 200,760 cases (
Figure 1). Estimated incidence rate was 0.055. Survival time of the diagnosis of adjustment disorder among cases in the 25th percentile was 2 months, meaning that for 25% of cases, the duration of time between the first and last observed treatment encounters related to adjustment disorder was 2 months or less. Survival time of the condition among cases in the 50th percentile was 8 months, and among cases in the 75th percentile, the condition lasted 28 months. In contrast, estimated 25th percentile survival time for any psychiatric diagnosis was 9 months, 50th percentile survival time was 21 months, and 75th percentile survival time was 47 months. Thus, although adjustment disorder diagnosis is transient, after 60 months of observation, 17.0% (95% confidence interval [CI]=16.8%–17.2%) of the sample (N= N=200,760 participants) initially diagnosed with adjustment disorder continued to present with at least one
ICD-9 adjustment, psychotic, mood, anxiety, or substance use disorder.
Table 1 and
Table 2 show improved balance across covariates after IPTW for the medication treatment and psychotherapy treatment groups, respectively. These tables are inclusive of 151,185 participants and highlight several differences in demographic and clinical characteristics for patients receiving medication or psychotherapy after receiving a diagnosis of adjustment disorder. Patients receiving medication as a baseline therapy were more likely to be female (0.7% versus 0.6%) and older (mean age 42.8 versus 36.4 years) and to have a higher burden of chronic illness (4.9 versus 4.2 conditions). In contrast, patients receiving psychotherapy were more likely to be male (0.4% versus 0.3%), younger (mean age 35.8 versus 44.5 years) and less likely to have chronic illnesses (3.8 versus 6.7 conditions). In addition, both medication and psychotherapy receipt were correlated with county-level characteristics, with higher urbanicity, population, psychiatrist-to-population ratio, and median incomes all favoring receipt of early psychotherapy instead of medication.
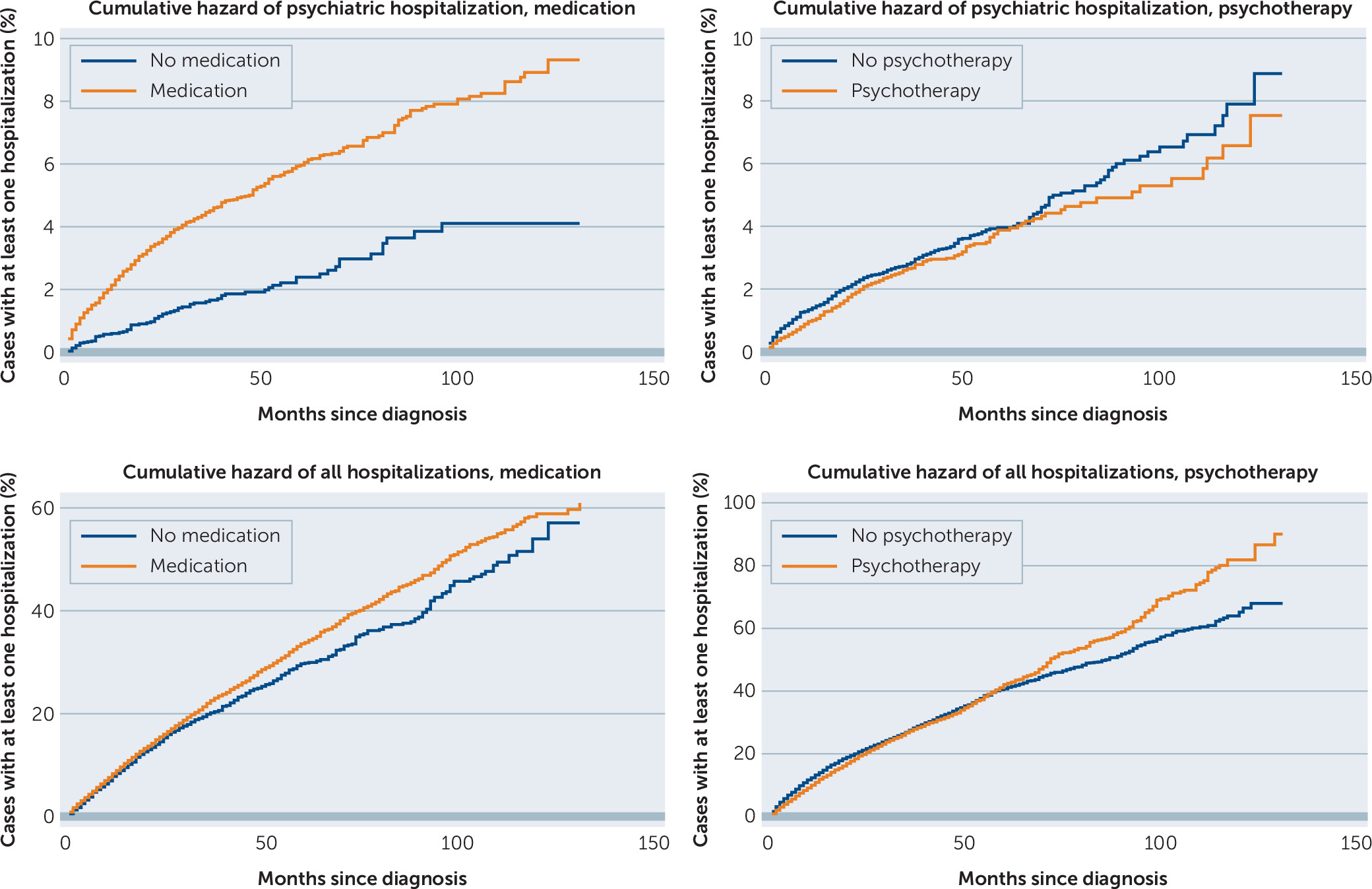
Table 3 presents the estimated hazard ratios of medication and psychotherapy on the outcome of hospitalization before and after fitting with IPTW. Receipt of medication within 1 month of diagnosis, with or without adjunct psychotherapy, was associated with an increased hazard of later psychiatric hospitalization (HR=2.61, 95% CI=2.07–3.28) but no difference in later hospitalization overall. In contrast, receipt of psychotherapy within 1 month of diagnosis was associated with a small decrease in hazard for later psychiatric hospitalization (HR=0.85, 95% CI=0.73–0.99) but no change in later hospitalization overall. Hazard ratios were observed from an incidence rate of 0.00073 per month (approximately 1% per year). The unweighted analysis for receipt of medication showed an association between early medication treatment and an increased hazard of later psychiatric hospitalization (HR=1.75, 95% CI=1.64–1.88) and for hospitalization overall (HR=1.37, 95% CI=1.33–1.41). For psychotherapy, there was no significant observed association with later psychiatric hospitalization in the unweighted sample, but a much lower likelihood for hospitalization overall (HR=0.48, 95% CI=0.47–0.50). Compared with the weighted samples, selection of treatment modality for adjustment disorder apparently varied on the basis of the patient’s physical health.
Cumulative hazard plots for the weighted analysis are displayed in
Figure 2, demonstrating higher cumulative hazards for the early medication group and lower cumulative hazard for the early therapy group in comparison with matched controls for the outcome of psychiatric hospitalization. Additionally, early medication treatment appeared to be associated with marginally higher rates of hospitalization overall.
Additional examinations looking specifically at psychiatric hospitalizations for patients receiving benzodiazepines were limited by the smaller sample (8,556 participants after caliper application). Both unweighted and IPTW estimates for benzodiazepine prescription found increased hazard of later psychiatric hospitalization (HR=1.67, 95% CI=1.51–1.85 and HR=1.59, 95% CI=1.02–2.51, respectively), although this finding was not higher than for medications overall. (See the online supplement for further details of the benzodiazepine analyses.)
Discussion
Chronicity in adjustment disorder was the first outcome of interest. Through this analysis of claims data, we estimated 5-year chronicity after adjustment disorder to be 17.0% (95% CI=16.8%–17.2%) of the sample (N=200,760 participants). In comparison, 5-year chronicity, as estimated in Andreasen and Hoenk’s sample (
7), suggested a 95% CI=16.3%–42.0%. Thus, there is potential to improve the precision of measurements from long-term follow-up through the use of epidemiological samples.
Our results suggest that patients who receive medication as a first-line treatment are more likely to be subsequently hospitalized than those who do not. Benzodiazepines, in particular, were associated with an elevated risk of later psychiatric hospitalization, although the difference in risk did not statistically differ from that seen with all medications as a group. In comparing aggregated unweighted to weighted estimates, it was notable that the inferiority of medication intervention was not driven by higher-risk patients disproportionately receiving medication rather than psychotherapy. If higher-risk patients had disproportionately received medication, then differences between groups would have been attenuated upon IPTW weighting. However, the findings indicated the opposite was true; that is, instead of treating patients with either medication or psychotherapy primarily on the basis of symptomatic severity, the variation in provider practice was more idiosyncratic.
Given that psychotherapy is generally recommended as the first-line treatment for adjustment disorder, it may be surprising that the first-line treatment choices of providers were so heterogeneous (
8). The results of our analyses suggest two possible explanations: treatment decisions for adjustment disorder may vary, in part, because of provider comfort and/or limited access to psychotherapy. For example, patients with higher general medical burden were far less likely to receive early psychotherapy. This result could be explained if either the providers were more comfortable with medications than with psychotherapy or if patients with general medical illness were reluctant to seek additional psychiatric care. However, the findings suggest that such practices may have deleterious effects for patients: after weighting the samples such that patients receiving psychiatric medications had on average fewer comorbid conditions than the control group cases, the medication treatment group remained at higher risk for hospitalization. Psychotherapy receipt was also strongly correlated with county-level characteristics, suggesting patients may also have received medication instead of psychotherapy because of limited local access to mental health services.
This study was observational in nature, and thus had some limitations. First, as with any propensity score analysis, estimated bias was maintained in the presence of omitted variables. For example, psychiatric severity was an omitted variable, although this limitation was ameliorated through the use of IPTW. Second, some residual imbalances remained after weighting. These covariate imbalances were allowed to remain because the covariates were generally biased in a direction opposing native selection. For example, if patients with more chronic illnesses are more likely to be hospitalized for psychiatric reasons at baseline and are also more likely to receive medication treatment, then reweighted groups including more chronically ill patients in the control group should favor the null hypothesis. Thus, although the estimated attenuation would affect our inference in the event of a null finding or of a reversal from the sign of the native correlation, it did not substantially affect interpretation of the study results as presented. Third, the study sample was extracted from private claims data. Because private insurance is more generous on average than public insurance, the description of practice heterogeneity observed here is not likely to be reiterated exactly. However, it is significant that even in private claims data, examples of geographic characteristics affecting care receipt persisted. Fourth, although type of psychotherapy data may be clinically informative for guiding the treatment of adjustment disorder, these data were limited in that the type of psychotherapy was not coded. Thus, we cannot comment on the relative efficacy of supportive, cognitive behavioral, psychodynamic, or other types of psychotherapy.
Conclusions
This study provides descriptive information regarding the chronicity of adjustment disorder as well as evidence that patients who receive psychotherapy as an early intervention may have better outcomes than patients who do not receive early intervention with psychotherapy. In contrast, patients who received medication as an early intervention were more likely to be subsequently hospitalized than those who did not receive medication as an early intervention. This analysis suggests that type of treatment may be at least partially driven by provider preference and severity of the patient’s general medical condition rather than by the severity of the psychiatric disorder alone. Given the prevalence of adjustment disorders in the population, these findings may provide some guidance for practitioners and reiterate the importance of access to specialty mental health care in determining the treatments that patients receive.