INTRODUCTION
This paper is concerned with potential variations between cultures in the meaning and meaningfulness of five different diagnostic categories in the substance use disorders: dependence, abuse, harmful use, intoxication and withdrawal. We are thus not concerned with differences between cultures in population rates of the diagnostic categories and of their criteria, but rather with prior questions of the meaningfulness and meaning of the criteria and diagnoses in different cultures.
There are two main traditions by which the issue of such cross-cultural variations has been addressed, primarily but not solely with reference to alcohol. One tradition starts from a position of universalism and philosophical realism, presuming that there is a single underlying dependence disorder applicable, for instance, to all humankind. The tradition may recognize problems in applying a diagnosis or instrument in a particular culture, but the solution to the problems lies in finding new operationalizations—the universal applicability of the underlying concept is not questioned. This has been the mainline position of American psychiatric epidemiology since the “St Louis revolution”, and it is probably difficult for many of us to set it aside and consider alternative perspectives.
The alternative tradition is more nominalist and particularistic, viewing substance use diagnoses as culturally influenced and allowing for the possibility that the cultural influence in framing the criteria or diagnoses can be strong enough that they are inherently different in different cultures. This tradition applies to the field of diagnostic concepts and instruments ethnographic perspectives on cultural variations in the meaning of substance use and intoxication as developed for alcohol, for instance, by MacAndrew & Edgerton (
1).
In his late writing about alcoholism, Jellinek was the first modern proponent of this way of thinking about substance use diagnoses. Jellinek was a thoroughgoing nominalist about what counts as a disease or disorder—more thoroughgoing than I would choose to be, for instance, when he said that “it comes to this, that a
disease is what the medical profession recognizes as such” (
2). His late definition expanded the frame of “alcoholism” so that it lost most of its specific meaning: “any use of alcoholic beverages that causes damage to the individual or society or both” (
2), and his Greek-letter types of alcoholism within this overarching frame essentially reflected the different “species” he had heard described as alcoholism by doctors from different countries at World Health Organization (WHO) meetings: gamma alcoholism was the “Anglo-Saxon” (i.e. American) species, delta alcoholism the French and epsilon the Finnish (
3).
THE FINDINGS OF EXISTING STUDIES ON CROSS-CULTURAL EQUIVALENCE AND VARIATION
In recent decades, there has been considerable research on the cross-cultural applicability of substance use disorder criteria and diagnoses, particularly for alcohol. Many of these studies have been framed in the paradigm of the realist and universalist tradition. For example, the book by Helzer & Canino (
4) on studies conducted with the Diagnostic Interview Schedule (DIS) instrument relies primarily on the fact of common methodology and that usable data could be produced as its warrants of comparability across a variety of studies (
5), but does include some side-comments about issues of applicability. Another study, a side-product of the WHO collaborative project which produced the Alcohol Use Disorders Identification Test (AUDIT), performed principal-component factor analyses in each of six diverse cultures of 13 alcohol dependence items covering aspects of impaired control, salience of drinking, tolerance and withdrawal (
6). The analysis found a strong general factor in each factor analysis, with very high Cronbach's alphas, and interpreted the results as support for “the hypothesis that the Alcohol Dependence syndrome has considerable cross-cultural generalisability, regardless of treatment ideology, culturally learned drinking patterns or societal response to drinking problems”. However, the paper also found that the dependence score formed from the items correlated quite highly with frequency of drinking 12 + drinks on an occasion (0.67–0.86) and with a logged score of alcohol-related personal, social and health problems (0.65–0.89). These findings are further evidence of cross-cultural commonality, but raise the question: commonality in what terms? Is it specifically the Alcohol Dependence syndrome which serves as the engine of the cross-cultural commonalities, or might it as well be the symptomatology of frequent intoxication or the experience of alcohol-related problems?
Another study was focused more specifically on assessing the validity of
Diagnostic and Statistical Manual (DSM) and
International Classification of Diseases (ICD) diagnoses cross-culturally, with test-retest and cross-instrument comparisons. However, the primary weight in the main round of published analyses from this study (
7,
8) was on analyses combining the different sites. The main site-specific comparative analysis in this series (
9) found substantial variation across sites in test-retest reliability, with Sydney, Australia showing the highest reliability on seven of nine current alcohol dependence items (Sydney range: 0.73–0.90). Bangalore, India showing the lowest on all nine items (Bangalore range: 0.29–0.53) and the results in Jebel, Romania closer to those for Sydney than those for Bangalore. Sydney and Jebel both also showed relatively high reliability on two alcohol abuse items, while again Bangalore showed lower reliability. Examining the patterns of discrepancies, the authors concluded that the Bangalore respondents appeared to have “difficulty understanding the constructs underlying the questions”.
The alternative tradition relies on a broader range of types of evidence, reaching outside the bounds of DSM or ICD instruments. Some of the evidence comes from quantitative studies in the realist/universalist tradition which, like Chatterji
et al. above, have sometimes produced findings which are problematic for the paradigm. Thus Klausner & Foulks (
10) were stimulated by the outrage of their subjects at the practical impact of their study (including an abrupt fall in the market value of the community's municipal bonds) to return to their data for a kind of after-the-fact protocol analysis of what their Inuit respondents could have meant in their answers to the items of the Michigan Alcoholism Screening Test (MAST) score. Somewhat ruefully, the authors concluded that many of the MAST items might well have a different meaning in an Arctic indigenous culture than, for instance, in urban Michigan. Applying the Munich Alcoholism Test (MALT) developed in Germany to samples in Spain and Ecuador, Gorenc
et al. (
11) found that five of the 31 items were “relatively free of cultural differences” by their criteria, but added that none of the five items as used in Ecuador passed the filters used to screen out items when the test was developed in Germany. Drawing on historical and anthropological studies, the present author argued 20 years ago (
12) that perhaps alcohol dependence should be viewed as a “culture-bound syndrome”, with a specific history and cultural inception which starts with the early American temperance movement (
13).
The most extensive study so far drawing on this more phenomenological tradition was the nine-site WHO study of the cross-cultural applicability of the substance use disorders (
14–
16). With limited resources and time for the data collection, the study's ambitious programme of key informant interviews, focus groups and reference case interviews was only partly carried out, and the analyses rely principally on the key informant interviews with knowledgeable local professionals and laypeople—20 at each site concerning alcohol concepts and terms and 20 concerning the drug with the highest apparent rate of harmful use at the site. The study identified problems of cross-cultural applicability at the level of instrument items, at the level of criteria, and at the level of concepts and diagnoses. Some problems at the item level were easily solved: phrases such as “driving an automobile or operating a machine” obviously require adaptation. Others were less tractable: it was noted that “the diagnostic criteria and their operationalizations assume a self-consciousness about feelings, knowledge and consciousness which is foreign to the folk traditions of some cultures” (
15). Thus there was no accurate translation in one or another society for words such as “feel” and “anxiety”. Items and criteria “often also have built-in attributional, causal and other relational assumptions which are not customary in some languages and cultures”. Thus formulations such as “trouble because of drinking”, “after you had realized it had caused you” and “where it increased your chances of getting hurt”, and items mentioning intentions presume “both self-consciousness and a style of causal attribution which is unrecognizable in some cultures” (
15). The problems posed by such items are not a mere problem of translation. Built into the DSM and ICD criteria are formulations which reach across and connect different domains of meaning. Thus, for instance, “the substance use continued despite knowledge of having a…problem that is likely to have been caused or exacerbated by the substance” is a criterion which requires connecting together acknowledgements of use, of a problem and of cognition about a causal relation between the two. The attribution of causality to alcohol and drug use, in particular, varies across cultures, and for that matter has varied in different periods within cultures (
16,
17). The study identified several different types of difficulty with the criteria for dependence. In some cultures there was no term for the criterion; in others the meaning of two criteria overlapped; while in others the criterion was not considered of diagnostic significance (
15).
In the context of categorical diagnoses and criteria, the issue of the threshold at which an item or criterion is considered positive becomes particularly important (
16). The WHO cross-cultural applicability study found many instances of different thresholds being applied. Where use of the substance is particularly suspect, the thresholds may be set very low. Thus in Bangalore, several reference cases qualified as positive on three or four alcohol dependence criteria on the basis of drinking a maximum of three drinks up to three times a month (
15). Conversely, in Athens and Santander, Spain, where regular drinking is normalized, thresholds for what is problematized were set much higher (
16). We may expect the same kinds of cross-cultural variation for other drugs according to the social acceptability and familiarity of the substance. Whether and how a threshold is defined is important in distinctions between normal drinking or drug use and harmful use or intoxication (
14), and between hangover and withdrawal (
15), as well for the criteria of dependence.
THE SOCIETAL FRAMING OF DIAGNOSIS
The issue of divergent thresholds brings to the fore the fact that clinical diagnoses in the alcohol and drug area, more than most other diagnoses, usually carry a weight of moral judgement, whatever the clinician's intentions. Of course, it is not that all use is always negatively evaluated. In most human societies, one or another psychoactive substance is a valued commodity for human ingestion. Human use values for psychoactive substances are varied (
18)—to ensure wakefulness, to promote sleep, to bring euphoria, to deaden pain, to pursue a transcendent experience, to quench thirst, as a nutrient, as a medium of commensality and sociability, as a signal of exclusion, and so on. The same substance often has apparently contradictory use values, sometimes simultaneously.
On the other hand, use of psychoactive substances beyond some socially defined limit (or, in some cases, at all) is commonly moralized and stigmatized. One has only to mention terms such as “drug fiend”, “demon rum” and the “scourge” or “menace” of drugs to recognize the extent to which drug use is often stigmatized. In many societies a common means of derogating opponents is to label them as drunks or drug users (
19); hence, as a policy of political prophylaxis, the ban on alcohol at the December 2004 encampments of the “orange revolution” in Kiev (
20). Another WHO study, of the cross-cultural applicability of disability concepts and measures in 14 societies, found some variation between societies in the ranking by informants of “alcoholism” and “drug addiction” in terms of degree of stigma (
21) (
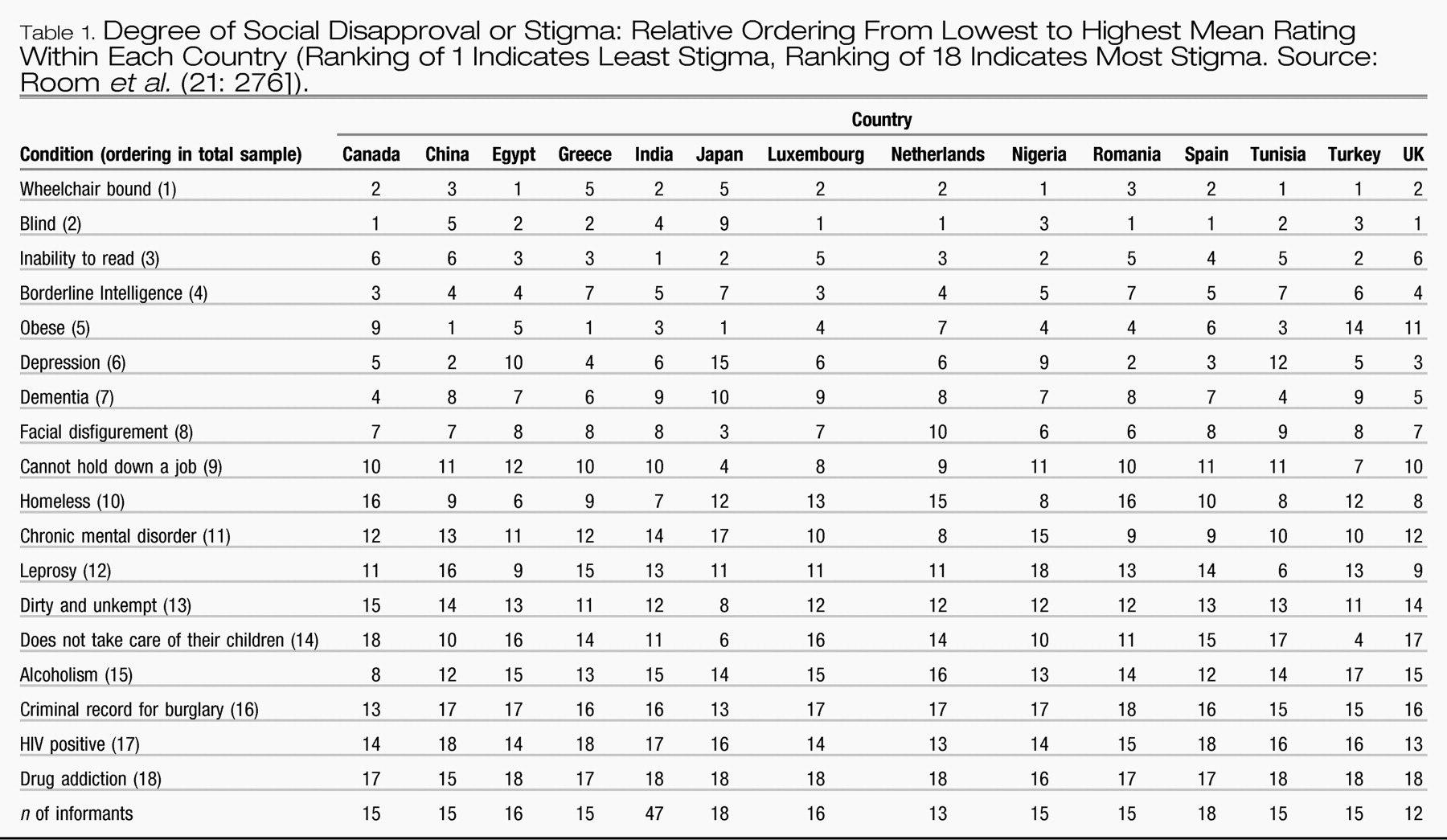
Table 1). However, the overall picture was that both conditions were ranked as among the most stigmatized of 18 conditions, roughly on a par with being “dirty and unkempt” and having a “criminal record for burglary”. The moralization of drinking or drug use, beyond thresholds that vary between cultures, seems to be one commonality we can find between many modern societies.
To a certain extent, the stigmatization is built into the diagnostic terminology of DSM-IV. This is most obvious in the use of the term “abuse”. Accordingly, in 1993 the Board of the American Society of Addiction Medicine, “while recognizing that ‘abuse’ is part of present diagnostic terminology”, recommended “that an alternative term be found for this purpose because of the pejorative connotations of the word “abuse”' (
22). It can be argued that the term “dependence” also came with some built-in stigma; when it was adopted in the 1960s and 1970s by World Health Organization committees it already carried a baggage of discreditable previous meanings in the United States, as in “dependent personality” or “welfare dependency” (
23).
Whatever diagnostic terminology is employed, the diagnoses are used primarily in clinical settings late in a process which begins in everyday life and interactions. Typically, for a majority of the cases coming into an alcohol- or drug-specific treatment service, someone—a spouse, another family member, a judge, a social worker—has made a judgement that there is a problem needing clinical attention. In fact, of those entering alcohol treatment in a California county, over 40% had received an ultimatum from someone to enter treatment, in 24% of the cases from a family member (
24). In such circumstances, a
de-facto part of the diagnostic decision-tree is the threshold at which family, friends or officials in the society notice a behavior and decide that it should be brought to professional attention. Often attached to these processes of “noticing”, as
Table 1 implies, is a great deal of stigmatization.
One decision for DSM is whether and to what extent a medical diagnostic system should build these essentially social judgements into the diagnosis and criteria, and to what extent it should seek to build diagnoses and criteria which are independent of them. This is the primary issue on which DSM-IV and ICD-10 parted company, with ICD-10's “harmful use” in principle excluding negative social consequences or reactions of others to drug use as evidence of harmful use (
25, p. 74–75], while DSM-IV's “abuse” was primarily built around them. I have noted that this divergence “reflects a longstanding difference between British and American psychiatry, with the British taking the view that social reactions and consequences do not belong in definitions of diseases and disorders” (
3). Behind this difference, I believe, lie not only differences about the inclusion of stigmatizing terms in the diagnostic system, but also the very different institutional frames of British and American psychiatry. In the context of the National Health Service, British psychiatry has been in a good position to define for itself the limits of its reach, with little to lose from turning away cases that fall outside those limits. In the absence of a national health system, the social environment of American psychiatry has been more entrepreneurial and less inclined to decide collectively that cases lie outside its competence. “A health system like the American, characterized by fee-for-service and managed care”, has encouraged inclusiveness in the criteria and thresholds, to make it “unlikely that a clinician will have to turn away anyone appearing for treatment on the grounds that they do not qualify for the diagnosis” (
3).
To the extent this judgement is right, it underlines that cultural differences in the nature of alcohol and drug problems which are presented to the health system reflect not only cultural differences in norms and behaviors around substance use, but also societal and cultural differences in how alcohol and drug problems are defined and handled. That is, the difference between the British and American views is not so much a reflection of differences in the nature of alcohol and drug use (in a global perspective, these differences are not very great) as it is of differences in the way that problems from the use are handled.
DSM started as a diagnostic manual for the United States, but it has obviously taken on a much broader significance. The efforts to conform the substance use diagnoses and criteria in DSM-IV and ICD-10 (
3) exemplify the fact that DSM has a global reach. In this context, it seems important to take into account that problem definitions and social handling systems for alcohol and drug problems differ considerably in different societies. For instance, to include “abuse” within the competence of psychiatrists and other clinicians may make sense in the context of the US system, with its strong interlinkage with the criminal justice system, but may make less sense elsewhere.
To take one example, in Sweden, where the general lay term for those with alcohol or drug problems translates as “misusers”, the primary institutional frame for alcohol and drug treatment (accounting for two-thirds of it) has long been the social welfare system, with the health-based system taking on specific tasks such as detoxification and opiate maintenance (
26). The Swedish system thus does not need a medical diagnosis of “abuse” to function. It is not that Swedish doctors ignore alcohol and drug problems: in fact, there has been a long tradition of concern by Swedish doctors about alcohol problems, but the fairly consistent theme for a century has been that, while there are medical aspects such as cirrhosis, the problem is primarily social in nature (
27).
WHAT MIGHT BE DONE?
For the following discussion. I take as one of my cues the comments by Marc Schuckit at a symposium on the validity of DSM-IV dependence, including the possibility of moving toward a dimensional approach (
28). Another cue is the fact that, by international treaty, national diagnostic systems must be based on the ICD, which means that a DSM classification has to be fitted within the frame of ICD diagnoses. The other cues for the discussion come from the findings of the studies of cross-cultural comparability:
•.
that the wording should avoid, as far as possible, causally attributive language; reference to feeling and affect states: combining different conceptual domains in the same item: and culturally specific circumstances or activities (except as examples); and
•.
that the threshold of any application should be specified; and in case of a dimensional approach, degrees of severity should be specified.
It is recognized that reference to feeling and affect states cannot be avoided for one of the diagnoses, dependence, discussed below.
My suggestions for directions of work are specified in terms of five current diagnoses (three shared by ICD-10 and DSM-IV, and harmful use from ICD-10 and abuse from DSM-IV).
INTOXICATION
The current DSM-IV criteria for intoxication are focused around behavior, rather than around extent of intake of the substance
per se. It is clear from the anthropological literature (
29) and from the qualitative cross-cultural studies (
15) that there are substantial cultural differences in what are regarded as signs of alcohol intoxication, reflecting differences both in amounts of drinking equated with intoxication and in cultural expectations and norms on behavior while intoxicated (
30). Similar variations can be expected for other psychoactive substances.
One clear choice here would be to move towards setting the intoxication diagnosis on a physiological basis, as a measure of recent ingestion of substantial amounts of the substance (or, in a dimensional approach, as a quantified measure of recent ingestion). In the case of alcohol, consideration for standard measurements to use should include not only interview questions (
31) and the familiar blood-alcohol measure, but also a diversity of biological measures which give quantified evidence of recent alcohol use (
32–
34). The extent to which such measures are available or can be developed also for other substances should be considered. The development of useful interview questions on quantity of intake of controlled substances has already been identified as a priority for the United States (
35).
A quantitative threshold or scale of intoxication is potentially a culture-free measure that is clinically relevant. There will, of course, be individual and culturally mediated differences in the behavior associated with the intoxication. As required, these could be measured separately, and then correlated to the intoxication measure.
WITHDRAWAL
The DSM criteria start with cessation or reduction of use of the substance, and a requirement of at least two (alcohol, amphetamines, cocaine, sedatives), three (opioids) or four (nicotine) physical or psychological signs, depending on the substance group. But there is also a third criterion, of “clinically significant distress or impairment in social, occupational or other important areas of functioning”. The “impairment” alternative in this criterion C obviously opens the door to a great deal of variation by culture and circumstance. Is it really desirable to have a particular state qualify as withdrawal on a working day, for instance, but not on a holiday, or not for a pensioner, as the “occupational functioning” subcriterion would imply?
In the WHO cross-cultural applicability study, withdrawal was as subject to cultural variation as the psychological symptoms (
16). The main issue was cultural variation in thresholds of severity, with those in the “wet” wine cultures inclined to set relatively low thresholds and no clear distinction from hangovers, and informants in cultures where drinking was viewed more problematically tending to give rather grave signs. Work is needed on developing specifications for thresholds for the different withdrawal signs which would reduce to a minimum cultural variation in the thresholds. It seems that, in principle, it should also be possible to develop biological measures of withdrawal, which would presumably further reduce the role of cultural variation.
HARMFUL USE (ICD-10)
This is defined as “a pattern of substance use that is causing damage to health” (physical or mental). The “diagnostic criteria for research” specify that “there must be clear evidence that the substance use was responsible for (or substantially contributed to) physical or psychological harm, including impaired judgement or dysfunctional behaviour, which may lead to disability or have adverse consequences for interpersonal relationships”, that “the nature of the harm should be clearly identifiable (and specified)” and that “the pattern of use has persisted for at least 1 month or has occurred repeatedly within a 12-month period”.
Harmful use has generally not performed very well in the test-retest studies (
36), and informants in the cross-cultural applicability study gave diverse characterizations of harm, often ranging well outside the limits of physical and mental health (
16). One problem with ascertaining harmful use from questions to patients or clients is that, of all types of harm, health harms are the most difficult for non-specialists to report validly (
37).
The best use of this diagnostic category, in my view, would be as a measure of patterns of heavy use over time (sporadic or continuous, say in the last 12 months) which carry a high risk of physical or mental harm. This may eventually be amenable to biological testing, but in the meantime could be captured by questions on patterns of heavy consumption (
31). Again there will be a need to specify threshold and levels.
Intoxication and harmful use would thus be a complementary pair, with intoxication measuring short-term (event-related) consumption, and harmful use measuring patterning of consumption over recent time.
It must be recognized that what is being proposed here is a version of hazardous use (
38), which was rejected as a diagnostic category in the ICD-10 decision process because it was not in itself a disorder. A partial way past this objection would be to specify levels of consumption at which physical or psychological damage is measurable.
SUBSTANCE ABUSE
This category has also generally not performed very well in test-retest studies (
36). It also does not hang together very well in terms of scaling (
8), although in my view there is no reason to expect the criteria which compose it to be held together more than by the fact of at least occasional heavy use of the substance involved.
The criteria for substance abuse deal with the realms of social roles and social and societal reactions to the substance user's behavior. Deciding on what would be the equivalents in terms of failure in work role for a shepherd and an airline pilot in a way that is culture-free seems difficult, to say the least. Furthermore, the criteria build in the societal reaction to the behavior, for instance in the “legal problems” of the third criterion, “expulsion from school” in the first criterion, and the “social or interpersonal problems” of the fourth criterion. An ambition to construct a measure of or criteria for “abuse” which will not be culture-bound thus seems fruitless. A further difficulty for cross-cultural comparisons is that causal connections are built into the criteria (“resulting in” in the first criterion, and “caused or exacerbated” in the third), and such conceptualizations caused difficulties in the cross-cultural applicability study.
A logical solution would be to transfer the recording of the phenomena now measured as abuse to Axes III and IV of the DSM system (mental problems would be coded elsewhere in Axis I). This would reflect the reality that the problems covered by the abuse criteria are mainly not health conditions in the usual sense. An alternative would be to retain a version of the substance abuse criteria with a notation that these criteria are developed for application only in US society, and other societies should develop their own culturally appropriate measures in this area. This alternative still begs the question, however, of whether such an “unwise” behavior as driving after drinking, which accounted for half the alcohol abuse cases in a US community sample, is treated appropriately as “a psychiatric disorder” (
39).
DEPENDENCE
The criteria for dependence received the most attention in the cross-cultural applicability study (
15,
16); as noted above, the study found a number of problems in their cross-cultural applicability. Essentially, the criteria bring together three conceptually different domains: physical dependence (tolerance and withdrawal), loss or impairment of self-control over substance use, and consequences of use. The consequences are explicit in the seventh criterion, which corresponds roughly to harmful use in ICD-10, and implicit to a varying extent in several others, most notably in the fifth: “a great deal of time spent in activities” around the substance, and the sixth; “important social, occupational or recreational activities given up or reduced because of substance use”.
My suggestion, in the light of the suggestions for the other diagnoses above, would be to “unpack” the present diagnosis and centre it around the related experiences of craving, feelings of compulsion and loss or impairment of control. That is, the core of the diagnosis would be composed from the third and fourth criteria in DSM-IV and the first in ICD-10 (“a strong desire or sense of compulsion to take the substance”).
Such a diagnosis, while still including a range of content, would be located solidly in the realm of the user's experiences and evaluations of his/her use. The greater conceptual coherence of the diagnosis would strengthen our ability to analyse the interrelations and contingencies of different aspects of substance use. It might thus give biological researchers a better target for their animal and other modelling. It would certainly map more readily onto public conceptions of addiction, alcoholism or dependence (
40).
Withdrawal would still be measured as a separate diagnosis. Tolerance turned out to be a difficult criterion in the cross-cultural applicability study (
15,
16); a number of different meanings were assigned to it, and in several places it was not considered to be associated with addiction. But if it was desired to keep tolerance diagnostically, it could perhaps be added in with withdrawal in a diagnosis of “physiological dependence” (although the term is now problematic, ironically in view of the term's history).
The fifth and sixth criteria (combined in a single criterion in ICD-10) are conditioned substantially by the social and cultural circumstances. Where the substance is readily and widely available (tobacco everywhere; wine in Spain), the issue of “time spent” seemed irrelevant to informants in the cross-cultural applicability study. The notion of “time spent” is also, to some degree, culturally conditioned; in Bangalore, “time was not viewed as a scarce or expendable commodity”. Giving up activities for drinking seemed irrelevant in Romania; it was remarked that “almost all pleasures are related to alcohol consumption” (
15). It is difficult to see how these criteria could be reformulated to be more culture-free.
In one sense, it can certainly be argued that a dependence diagnosis reformulated around the experience of impairment or loss of control and related concepts would also be culturally conditioned. Certainly, the argument that addiction concepts have a specific temporal and cultural history (
12) implies that there are times and places where such concepts would not be meaningful. Here, for example, are Kunitz & Levy (
41) describing the change in Navaho culture by which an addiction concept became meaningful: 19th century Navaho drinkers did “not for the most part define themselves as sick in the same way as health professionals do. As the society changes, however, these behaviors increasingly come to be seen as maladaptive to the new world where people are expected to be at work on time; where no network of kin is available to help when a husband is out drinking; where bills must be paid; and where all sorts of obligations the dominant society takes for granted must be fulfilled…. In the new society that is emerging, older patterns of behavior are increasingly defined as in some way deviant. The drinker's behavior comes to be defined as sick. He is no longer a man who drinks a lot; he is an alcoholic' (pp. 254–5).
By now, however, an addiction or dependence concept is now broadly used in much of the world, although there are certainly culturally specific nuances in its meaning. The criteria suggested here for the diagnosis are not directly dependent on interpersonal and social reactions. The desire to cut down or the intention to limit use may indeed be influenced by the wishes or mandates of others, but the wishes or mandates are not built into the criteria themselves. Instead, the criteria are organized around the user's own cognitive and affective experiences with respect to his or her use.
In revising the actual criteria for the diagnosis, attention might be paid to experience not only with the diagnostic instruments but also with various relevant assessment measures, such as the Alcohol Craving Questionnaire and the Impaired Control Scale (
42).