Modern electrophysiological methods of investigation allow the estimation of night sleep quality (polysomnography; PSG
1), daytime alertness (Maintenance of Wakefulness Test; MWT
2) and daytime sleepiness (Multiple Sleep Latency Test; MSLT).
1–3 Although these tests have been used in many investigations, data concerning the relationships between sleep structure, sleepiness, and alertness are contradictory. No strong relationships have been found between the MSLT results and sleep parameters.
4–8Akerstedt and Folkard
9 found negative relationships between subjective sleepiness and alertness, whereas subjective alertness correlated negatively with alpha power density. In patients with excessive daytime sleepiness, the positive correlation between MSLT and MWT accounts for less than 17% of the variability in these measures.
10 This means that some patients with abnormally low MSLT scores (i.e., greater readiness to fall asleep) were able to stay awake for a long time when asked to do so on the MWT. In narcolepsy, 82% of patients were concordant for the two tests, but 18% had high MWT scores (i.e., greater alertness) despite low MSLT results.
10 When motivated, some narcoleptics are able to maintain wakefulness.
1 In idiopathic hypersomnia, where 48% of patients were concordant for the two tests, 37% demonstrated low MSLT and high MWT scores. In sleep apnea, 70% of patients were concordant for the two tests, 15% demonstrated low MSLT and high MWT scores, and 15% had high MSLT and low MWT (inability to fall asleep and difficulty in staying awake). In depressed patients who complain of being tired and sleepy, concordance between tests results was found in 65% of patients, whereas 25% of patients could not fall asleep early (high MSLT) and also could not stay awake for a long time (low MWT).
10,11 The lack of correlation between MWT and MSLT was shown also in several other investigations.
6,12How can one interpret these data? From our point of view, the lack of correlation between sleep latency on MSLT and MWT is a very natural finding in healthy subjects when the sleep latency on MSLT is lower than the sleep latency on MWT. Healthy subjects without emotional and sleep disturbances, when motivated to go to sleep in the appropriate conditions (dark and noise-free environment) are often able to achieve stage 1 sleep in a relatively short period (in 10 minutes, according to MSLT). This means that their sleep-promoting brain mechanisms are not altered. On the other hand, when motivated not to sleep, healthy subjects demonstrate the ability to maintain wakefulness for a long time, because they are not sleep-deprived and their wakefulness-promoting brain mechanisms are also not disturbed. This approach corresponds to the observations by our group and others,
7,8,10,13–15 which emphasized that MWT and MSLT are measuring different abilities. In this construct, the better the nighttime sleep, the greater the daytime alertness as reflected in increased latency on MWT. However, sleep latency on MSLT may not increase in parallel with MWT sleep latency. To be healthy means to be flexible, to relax, and to be alert according to the requirements imposed by the environment—whereas the propensity to fall asleep may be indexing a different capacity.
In patients with excessive daytime sleepiness caused by impairment of the wakefulness-promoting brain mechanisms, as in the case of narcolepsy, it is reasonable to predict the high concordance between the two tests as was shown.
11 Sleep latency is decreased even when subjects are required to stay awake. When brain mechanisms in narcolepsy are relatively less impaired, additional motivation can increase sleep latency on MWT.
1 However, the opposite never occurs: sleep latency in conditions promoting sleep (MSLT) is never less than on MWT. On the other hand, if idiopathic hypersomnia is caused by the excessive activity of the sleep-promoting brain mechanisms, it is explicable that these patients often demonstrate low MSLT and high MWT.
11 The potential to mobilize mechanisms of alertness is still high in these patients. Sleepiness caused by the partial sleep deprivation that occurs in sleep apnea can be construed as a compensatory sleepiness based on the increased activity of the sleep-promoting brain mechanisms. Such sleepiness can be accompanied by the relatively high sleep latency on MWT.
12Another reason for the discrepancy between MSLT and MWT data may be a high maladaptive emotional tension caused by neurotic anxiety and/or depression.
16,17 As opposed to normal anxiety (adaptive emotional tension), which mobilizes subjects to solve problems, overcome obstacles, and achieve goals, maladaptive emotional tension is neither goal-oriented nor flexible. It persists without any pragmatic reasons and may increase alertness inappropriately.
16 As a result, it may induce insomnia.
18–20 Sleep disturbances caused by the maladaptive emotional tension may lead to increased subjective sleepiness and impair goal-oriented and consciously controlled attention. However, the same maladaptive emotional tension prevents normal sleep during the day
and during the night. This state may be in contrast to the increased sleepiness after partial sleep deprivation (as in sleep apnea). As a result, a very strange picture may appear: the more disturbed the nighttime sleep (that is, the higher the maladaptive emotional tension), the longer the sleep latency on MSLT. Sleep latency on MWT may also increase if the instruction to maintain wakefulness increases the emotional tension.
These considerations led us to hypothesize that the presence of maladaptive emotional tension has disruptive effects on normal sleep and alertness behaviors. These effects in turn could account for certain inconsistencies in previous studies of daytime alertness in different disorders.
The aim of the present study was to investigate this hypothesis by comparing relationships between sleep structure, MWT, and MSLT data in two groups of patients: those with depression/anxiety and those with sleep apnea without depression/anxiety. We predicted that correlations between sleep structure, MWT, and MSLT would be different in the two clinical groups. We hypothesized that in sleep apnea, sleep latency during the day would correlate negatively with night sleep disturbances, and that in depression such relationships would be absent.
METHODS
Subjects comprised 22 consecutive depressed patients (11 males, 11 females; mean age 42.6±13.5 years) and 47 consecutive nondepressed apneic patients (34 males, 13 females; mean age 49.2±14.4 years) attending the Sleep and Alertness Clinic for assessment of their sleep disturbances. The diagnosis of depression was based on the clinical assessment according to DSM-IV criteria. None of the patients were taking psychotropic medications. All of the patients scored high on depression and anxiety scales (Center for Epidemiologic Studies Depression Scale,
21 Zung Anxiety Scale,
22 Rosenberg Scale
23); however, none of these patients was diagnosed as having anxiety disorder per se. All apneic patients had low scores on the aforementioned scales. Patients were selected if they 1) met standard criteria of sleep apnea and were not depressed on clinical interview by DSM-IV criteria, or 2) met DSM-IV criteria for depression and did not show evidence of sleep apnea on polysomnography.
All patients underwent two consecutive overnight polysomnographic studies followed by the Multiple Sleep Latency Test and Maintenance of Wakefulness Test on the following days. The diagnoses of depression and apnea were supported by nocturnal polysomnography.
A standard PSG montage included electroencephalographic (C3 and C4 leads), electromyographic, and electro-oculographic monitoring. Respiration (oxygen saturation and number of respiratory events) and periodic leg movement were also recorded.
For the objective assessment of daytime sleepiness, the most widely used procedure, MSLT, was carried out following the first-night sleep study.
24 This procedure comprises 4 or 5 nap opportunities given every 2 hours in the sleep laboratory settings. The patients lie in a darkened, sound-attenuated room for 20 minutes and try to fall asleep. The time taken to fall asleep is objectively measured with the recording montage that was affixed the previous night. The average latency to sleep onset over all nap opportunities provides an index of sleep propensity. A smaller number reflects greater level of sleepiness; an average latency of less than 5 minutes indicates excessive daytime sleepiness.
Following the second-night sleep study, a related yet different procedure, MWT, was performed to measure objective daytime alertness. The MWT challenges the patient's ability to remain awake during soporific circumstances.
1,2 This test is administered similarly to the MSLT. The major distinctions are that in the MWT, the patient is
seated in a dark room and
instructed to remain awake. The MWT is also used for the assessment of treatment efficacy in disorders of excessive daytime sleepiness.
The overnight PSG recordings (138 in total) and daytime tests (69 MSLT and 69 MWT) were scored by experienced technologists according to standardized criteria.
25 Using the SPSS statistical software package for Windows, we analyzed the interrelationships among MSLT, MWT, and the preceding night's sleep variables, including total sleep time (TST), sleep efficiency (SE), sleep onset latency (SOL) and percentage in each sleep stage. Nonparametric analysis using the Spearman correlation coefficient and Mann-Whitney
U-test was performed.
26,27RESULTS
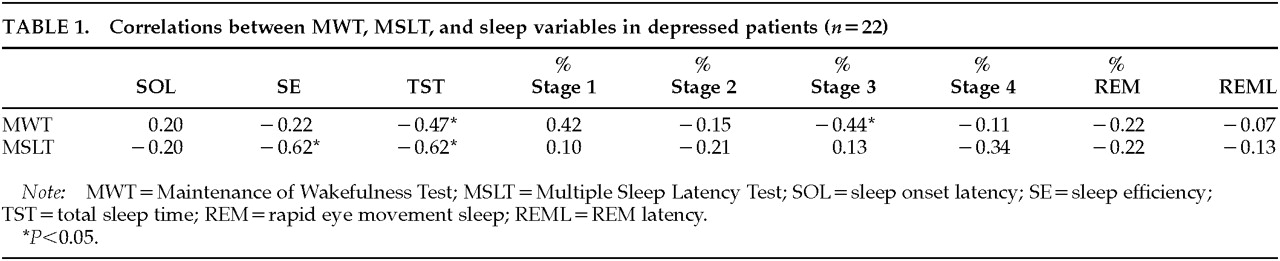
Interrelationships between MWT, MSLT and sleep variables in depressed patients are presented in
Table 1.
In depressed patients, MWT results correlated negatively with TST (–0.47, P<0.05) and stage 3 (–0.44, P<0.05). There was a positive correlation between MWT and percentage of stage 1 sleep; however, it did not reach the level of significance. MSLT results correlated negatively with TST (–0.62, P<0.05) and SE (–0.62, P<0.05). There was a negative correlation between percentage of REM (rapid eye movement) and stage 1 sleep (–0.48, P<0.05). REM sleep latency correlated negatively with percentage of REM sleep (–0.72, P<0.01). A negative correlation was also observed between the amount of slow wave sleep (SWS) and percentage of stage 1 sleep in depressed patients (–0.46, P<0.05). There was a positive correlation between SWS and TST (0.44, P<0.05).
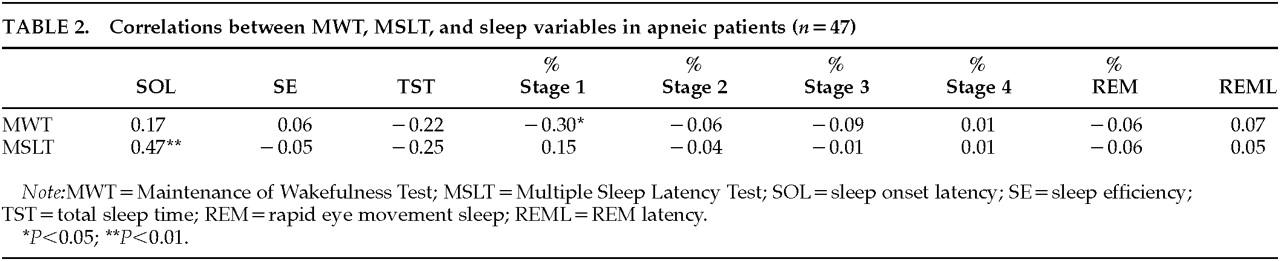
Interrelationships between MWT, MSLT and sleep variables in apneic patients without depression/anxiety are presented in
Table 2.
As opposed to the depressed patients, the sleep apnea group showed a significant negative correlation between MWT results and percentage of stage 1 sleep (–0.30, P<0.05). MSLT results correlated positively with SOL on the preceding overnight sleep study (0.47, P<0.01). Amount of stage 1 sleep correlated negatively with TST (–0.32, P<0.05), SE (–0.37, P<0.05), and SWS (–0.47 P<0.01). There was a positive correlation between percentage of stage 1 sleep and REM sleep latency (0.35, P<0.05). The latter correlated negatively with percentage of REM sleep (–0.53, P<0.01), SE (–0.41, P<0.01) and TST (–0.39, P<0.01). There was a positive correlation between REM sleep latency and percentage of stage 1 sleep (–0.35, P<0.05). SE correlated positively with TST (0.62, P<0.01) and SWS (0.50, P<0.01).
DISCUSSION
The main result of the present investigation is the finding of a significant difference between depressed patients and patients with sleep apnea vis-à-vis the relationships between sleep, alertness, and sleepiness. In depressed patients, sleep latency on the MWT increases in parallel with the night sleep disturbances; in sleep apnea, this does not occur. Moreover, in sleep apnea, relationships are opposite: MWT correlates negatively with stage 1, and stage 1 correlates with sleep disturbances (negatively with sleep duration and sleep efficiency). This means that the more disturbed nighttime sleep is in sleep apnea, the more difficult it is for patients to maintain alertness. Usually, Spearman correlations do not allow one to make any suggestions concerning cause-and-effect relationships. This investigation is an exception. The underlying reason for sleep apnea is well known, namely breathing disturbances during sleep. It is possible to assume that impaired alertness is determined by the disturbed sleep. This state corresponds to the impaired alertness after artificial sleep deprivation in healthy subjects.
28 The disturbed sleep quality in sleep apnea explains the positive correlation between MSLT and sleep onset latency on the preceding night: a common reason—increased sleep requirement caused by disrupted nocturnal sleep—determines the decreased sleep latency during the day and during the night. Negative correlation between REM sleep latency and sleep efficiency implies that in patients with sleep apnea, REM sleep latency is increased due to the awakenings in the first cycle. This feature is a hallmark of sleep apnea, indicative of the poor sleep quality in sleep apnea patients.
In depression, nocturnal sleep disturbances are not associated with increased sleepiness. To the contrary, the worse the sleep quality, the longer the sleep latency on MSLT and MWT. Thus, it is possible that the same factor causes night sleep disturbances and prevents sleepiness during wakefulness. This result confirms our initial hypothesis that the relationships between night sleep and alertness/sleepiness are different in patients with depression and with sleep apnea. Our findings suggest that depression/anxiety could be a moderating variable that may explain inconsistencies in the results of previous studies of alertness. It is possible to speculate that it is a maladaptive emotional tension that decreases night sleep efficiency, increases stage 1, and increases sleep latency on MWT and MSLT in depression. Thus, the quality of alertness in depression must be different from the quality of alertness in sleep apnea. It is our assumption that alertness can be subcategorized into two types: a maladaptive alertness as seen in depression/anxiety and probably associated with poor performance, and an adaptive alertness without impaired daytime functioning. This hypothesis requires further investigation.