When obsessive-compulsive (OC) symptoms coexistent with schizophrenia, the illness is referred to as obsessive-compulsive schizophrenia or schizo-obsessive disorder.
1 Recently, OC schizophrenia has been a subject of intensive research. Currently, there are two competing hypotheses concerning the role of OC symptoms in schizophrenia. One hypothesis claims that in the prodromal stage of the first episode of schizophrenia, OC symptoms may play a protective role against the onset of schizophrenic symptoms.
2 Another theory suggests that OC-schizophrenic patients are more impaired, both clinically and neuropsychologically, than schizophrenics who do not experience OC symptoms. The evidence for the latter is taken primarily from studies with chronic schizophrenia.
3The relationship between the neuroanatomical and neuropsychological mechanisms underlying schizophrenia and/or obsessive-compulsive disorder (OCD) is complex. While frontal lobe pathology has been evidenced in both disorders, functional neuroimaging generally points to a prefrontal hypoactivity in schizophrenia
4 and increased metabolic activity of prefrontal cortex in OCD.
5 Neuropsychological tests reveal that impaired performance connected with frontal lobe function is present in both schizophrenia and OCD, but more so in schizophrenia, linking this illness to the intensity of negative symptoms.
6–8 However, in a recent study conducted by Hwang et al.,
3 schizophrenic patients with OC symptoms scored worse than schizophrenics without OC on the Wisconsin Card Sorting Test (WCST). Patients with symptoms of OC were found to have frontal lobe activity and a higher degree of negative symptoms.
Frontal lobe pathology is a part of both schizophrenia and OCD, but the underlying neural circuits may involve different structures and different neurotransmitters. A circuit responsible for cognitive dysmetria is thought to effect schizophrenia,
9 while in OCD, it is believed that basal ganglia play a prominent role.
10 A dopaminergic deficit in frontal cortex may underlie hypofrontality in schizophrenia,
11 while serotonergic disturbance is believed the most significant cause of OCD, which has immediate therapeutic implications.
12The purpose of this study is to better elucidate OC syndrome in schizophrenia by comparing the performance on selected neuropsychological frontal lobe tests of carefully matched schizophrenia patients with or without OC symptoms (patients with “pure” OCD and control subjects).
METHODS
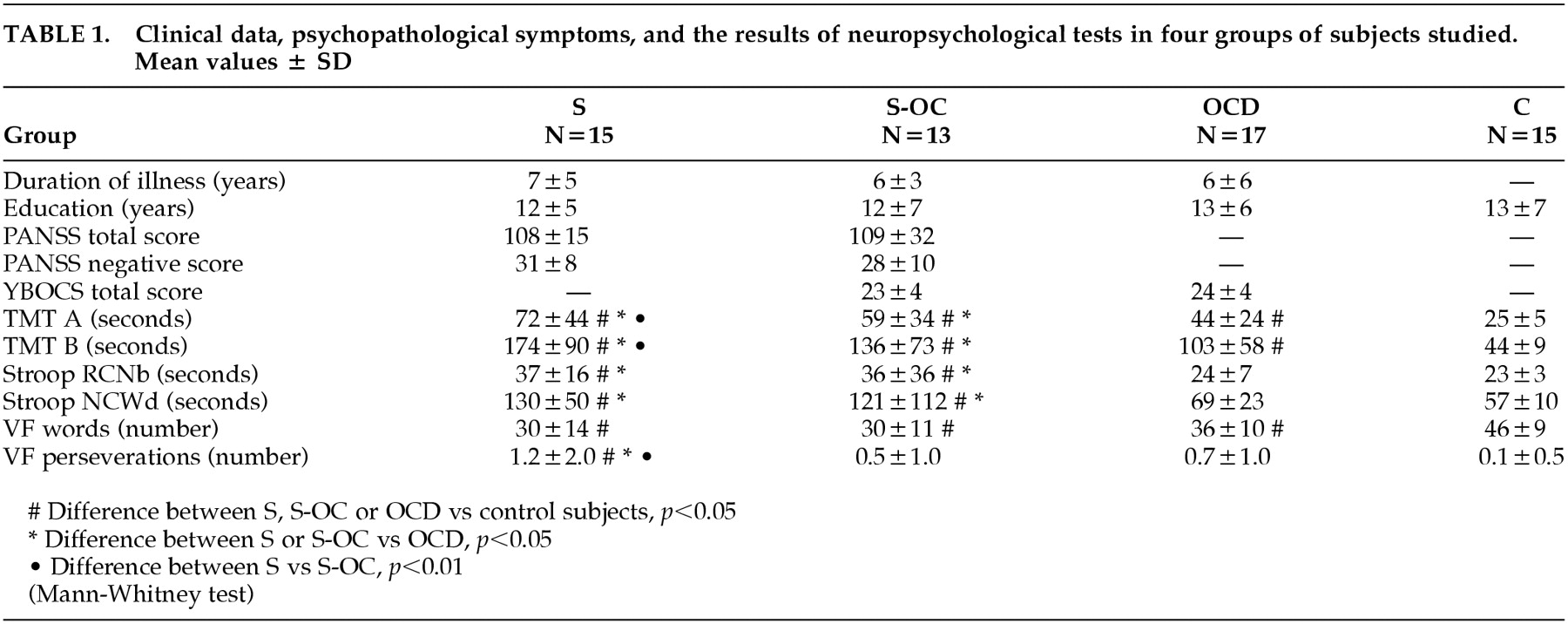
The study included 60 subjects divided into four groups (
Table 1):
Fifteen schizophrenic patients without OC symptoms (S), 8 male, 7 female, age 33+10y;
Thirteen schizophrenic patients with OC symptoms (S-OC), 8 male, 5 female, age 26+6y);
Seventeen patients with OCD, 10 male, 7 female, age 29+9y; and
Fifteen healthy control subjects (C), 6 male, 9 female, age 30+9y
Informed consent was obtained from all subjects, following a complete description of the procedure. All patients were treated at the inpatient or outpatient unit in the, Department of Psychiatry, University School of Medicine in Bydgoszcz, Poland. None of the patients had a history of substance abuse, neurological illness, or serious somatic illness. The diagnoses were made by psychiatric staff, using ICD-10 and DSM-IV criteria. All patients from group 1 and group 2 met the criteria for schizophrenia, and patients from group 2 fulfilled the additional criteria for OCD. OCD was the primary diagnosis for patients in group 3, none of which had concomitant psychiatric comorbidity (“pure” OCD). Control subjects were recruited from clinical staff or medical students. They were somatically healthy, and neither they nor their first-degree relatives had psychiatric or neurological illnesses.
Psychometric assessment of the intensity of schizophrenic symptoms was done using the Positive and Negative Symptoms Scale (PANSS), while the assessment of OC symptoms was conducted using the Yale Brown Obssessive-Compulsive Scale (Y-BOCS). At the time of investigation, all patients showed a moderate exacerbation of symptoms.
The assessment of cognitive functions was performed using selected neuropsychological tests:
•
The Trail Making Test (TMT). Part A of the test measures psychomotor speed and attention, Part B measures the ability to shift strategy and assess executive function and visuospatial working memory, reflecting the activity of frontal lobes
•
The Stroop Color-Word Interference Test. The first part of the test, Reading Color Names in black (RNCb), measures verbal abilities and attention; and the second part, Naming Color of Word–different (NCWd), measures such frontal lobe functions as verbal working memory and executive functions
•
The Verbal Fluency (VF), “FAS” Oral Word Association Test. This is a sensitive measure of executive frontal functions because it requires the subject to generate its own strategy. Assessments were conducted using the Polish version of the FAS: a number of words and a number of perseverations were scored
RESULTS
Table 1 shows clinical data, the intensity of psychopathological symptoms, and the results of neuropsychological tests in four groups of subjects studied.
Differences between groups regarding the duration of illness and level of education were not observed. Schizophrenic patients with or without OC symptoms had a similar intensity of symptoms, as measured by the PANSS scale (total and negative symptoms). Additionally, no difference in the intensity of OC symptoms measured by the Y-BOCS was found between patients with OCD and patients with schizophrenia accompanied by symptoms of OC.
On each test, the neuropsychological performance of all three patient groups was significantly poorer than that of control subjects. In TMT A tests and TMT B tests, a significantly improved performance was observed in OCD patients, as compared with both groups of schizophrenic patients (with or without OC symptoms). Among schizophrenic patients, however, those who had symptoms of OC performed better.
On the Stroop test, significant differences between OCD patients and healthy subjects were not found, and no significant differences were observed between schizophrenic patients with or without OC symptoms. However, schizophrenic patients had significantly worse results compared with OCD patients and control subjects, especially in Part B of the test.
All investigated patient groups demonstrated lower verbal fluency performance than healthy control subjects. Among schizophrenic patients, perseverations scores were worse in those without OC symptoms.
DISCUSSION
The performance of all three subject groups was significantly worse than that of healthy control subjects. These results are comparable with other neuropsychological studies that underscore frontal pathology in both schizophrenia and OCD.
6–8 However, on all assessments that were conducted, patients with OCD performed significantly better than patients with schizophrenia.
On tests measuring frontal lobe function, comparison of schizophrenic patients with or without OC symptoms revealed that OC schizophrenics scored either better than (TMT B, perseverations in VF) or similar (Stroop B) to schizophrenic patients without OC symptoms. Therefore, the main finding of our study reveals that, if groups of patients are matched for level of education and duration of illness, S-OC patients will show that they fall between “pure” schizophrenia and “pure” OCD, as identified on frontal lobe tests. This finding corroborates the results of studies that show some “protective” effect of OC symptoms on frontal impairment in schizophrenia.
2 In recent molecular genetic studies, common predisposing genes were postulated for both schizophrenia and OCD in S-OC patients; thus, a possibility for the comorbidity of these illnesses exists.
11,13To reconcile our findings with those of Hwang et al.,
3 we propose that the effect of OC symptoms (or OCD comorbidity) in schizophrenia may depend on the stage of the illness. In the early stage of schizophrenia, OC symptoms may have an alleviating effect. The Poyurovsky et al.
2 study included first-episode schizophrenic patients. The mean duration of illness in subjects used in our study was 7 years. The duration of illness in participants of the Hwang et al.
3 study was not given but may have been much longer than 7 years because chronic schizophrenic patients were included. It is possible that during chronic course, the (untreated) OC symptoms may further add to the deterioration of the clinical picture of schizophrenia. We could also speculate that early treatment of OC symptoms in schizophrenia may have a beneficial effect on the longitudinal course of the illness.