I n his initial monograph, Wilson described the behavioral aspects in eight out of the 12 patients with Wilson’s disease (WD), which he called “Psychical.”
1 As many as one third of these patients present with psychiatric and behavioral abnormalities and there are reports that all patients with Wilson’s disease have psychiatric symptoms.
2 Scheinberg and Sternlieb stated that every patient with Wilson’s disease suffers from one or more of the following problems at some point during the course of illness: organic dementia, psychosis, psychoneurosis, and behavioral disturbances characterized by impulsivity occasionally extending to unlawful behavior.
3 There are no such studies from India, except for a solitary case report.
4 The present study describes the psychiatric comorbidities in patients with Wilson’s disease, using Structured Clinical Interview for DSM-IV Axis-I Disorders-Patient Edition (SCID).
Subject and Methods
Fifty patients were recruited from a specialty clinic for Wilson’s disease at the Department of Neurology at the National Institute for Mental Health and Neurosciences in Bangalore, India, a tertiary care university hospital of south India. This was a heterogeneous sample with reference to gender, age group, educational and socioeconomic background, duration and severity of illness, and treatment. Their diagnosis had been established after the initial clinical suspicion by presence of Kayser-Fleischer ring on slit-lamp examination, low serum copper and ceruloplasmin levels, and increased 24 hours urinary copper. Clinical details were recorded in all.
Psychiatric comorbidity was assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID). SCID was administered to each patient by two psychiatrists independently, trained for SCID interview (SA, TM). The SCID is a semistructured diagnostic interview, which begins with a section on demographic information and clinical background. There are seven diagnostic modules focusing on different groups: mood, psychosis, substance abuse, anxiety, somatoform, eating and adjustment disorders. It is unique as it secures reliable information in different cultural settings. This study explored the psychiatric comorbidity in Wilson’s disease by administering structured clinical interviews in a systematic way.
RESULTS
There were 29 males and 21 females. The mean age at onset of symptoms was 14.2 ± 6.4 years (range: 5 to 37 years), and the mean age at diagnosis was 16.3 ± 7.0 years (range: 6 to 40 years). At the time of evaluation for psychopathology, the mean duration of illness was 10.4 ± 8.7 years (range: 1 to 50 years). The mean duration of de-coppering treatment with penicillamine (250 to 1000 mg/day) and zinc (180 mg/day) was 8.2 ± 7.3 years (range: 1 to 40 years). Three patients had positive family history in an autosomal recessive pattern. History of detailed psychiatric symptoms in the family was not available.
All patients except two had bilateral Kayser-Fleischer rings on slit-lamp. The predominant presenting manifestations in these cases could be categorized as neurological (25), psychiatric (6), hepatic (5), hepatic and neurological (4), osseomuscular (3), neurological and psychiatric (2), and neurological and osseomuscular (2). Three subjects were asymptomatic siblings of index patients. The mean level serum copper was 50.0 ± 46.7 μg/dl (range: 5 to 304 μg/dl), serum ceruloplasmin was 6.8 ± 6.0 mg/dl (range: 1 to 36 mg/dl), and 24 hours urinary copper was 425.1 ± 362.5 μg/dl at the time of diagnosis.
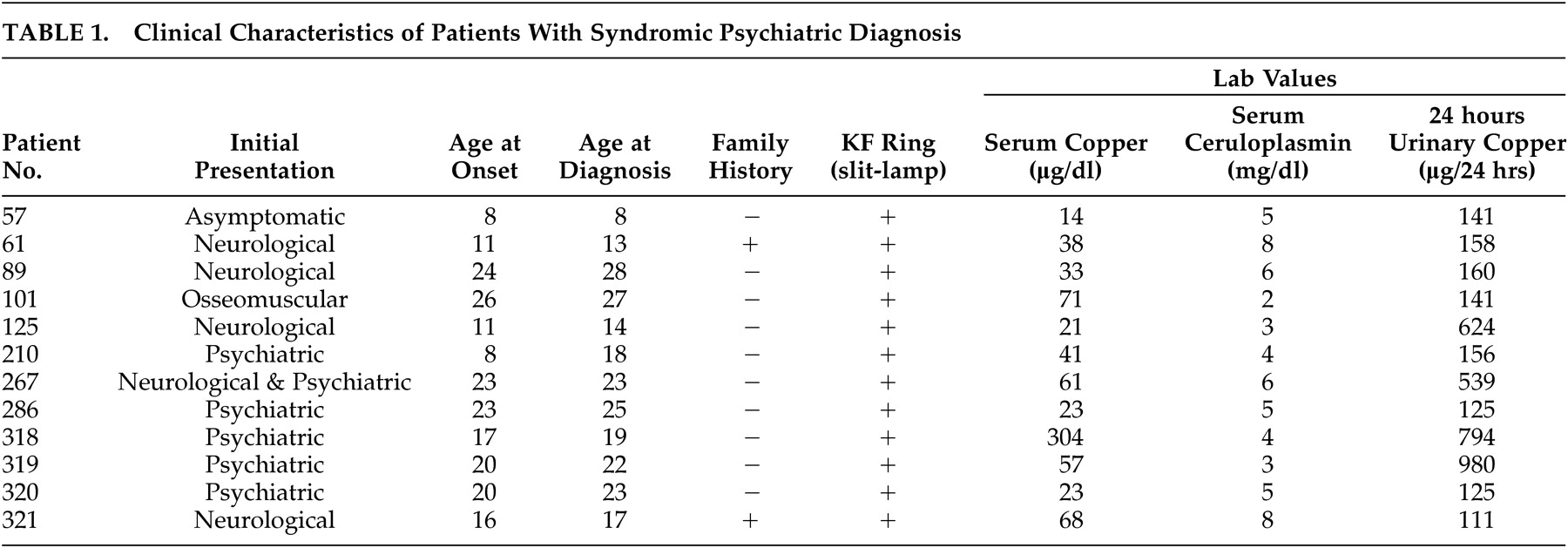
The key psychiatric symptoms in these patients were excessive talkativeness, aggressive behavior, loss of interest in the surroundings, and abusiveness. Twelve patients (24%) fulfilled the diagnostic criteria for syndromic psychiatric diagnosis with majority having affective disorder. Nine patients had bipolar affective disorder, two were diagnosed with major depression, and one had dysthymia (
Table 1 ). The age at onset of Wilson’s disease in patients with (N=12) and without (N=38) behavioral changes was not different (student t test: p=0.5). Psychiatric manifestations dominated the clinical profile in eight patients at the time of diagnosis, and all had BPAD at the time of evaluation. The neurological manifestations at the time of diagnosis included dystonia (8), speech disturbances (22), tremors (15), chorea (1), gait disturbances (10), seizures (2), and drooling (6).
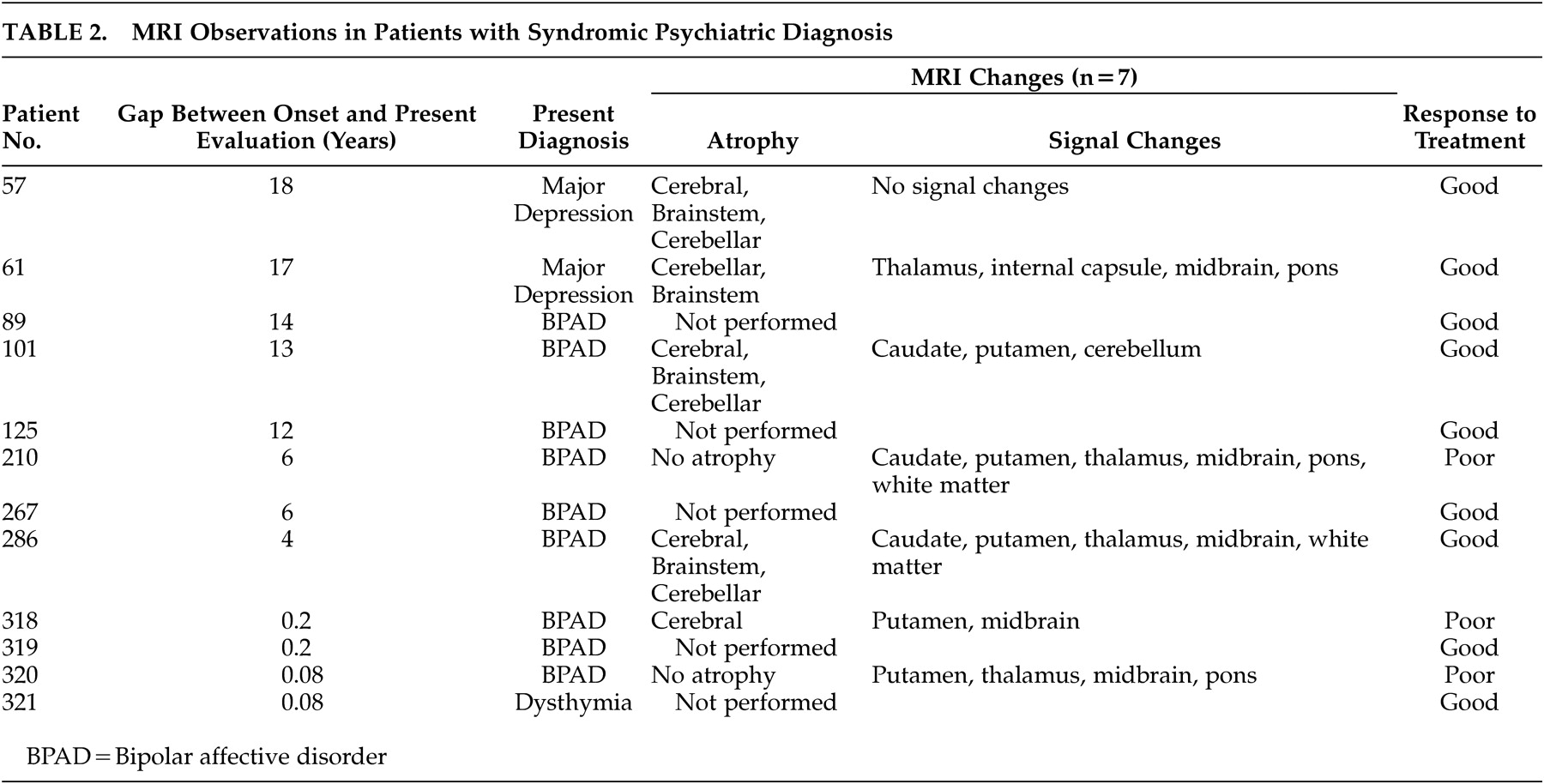
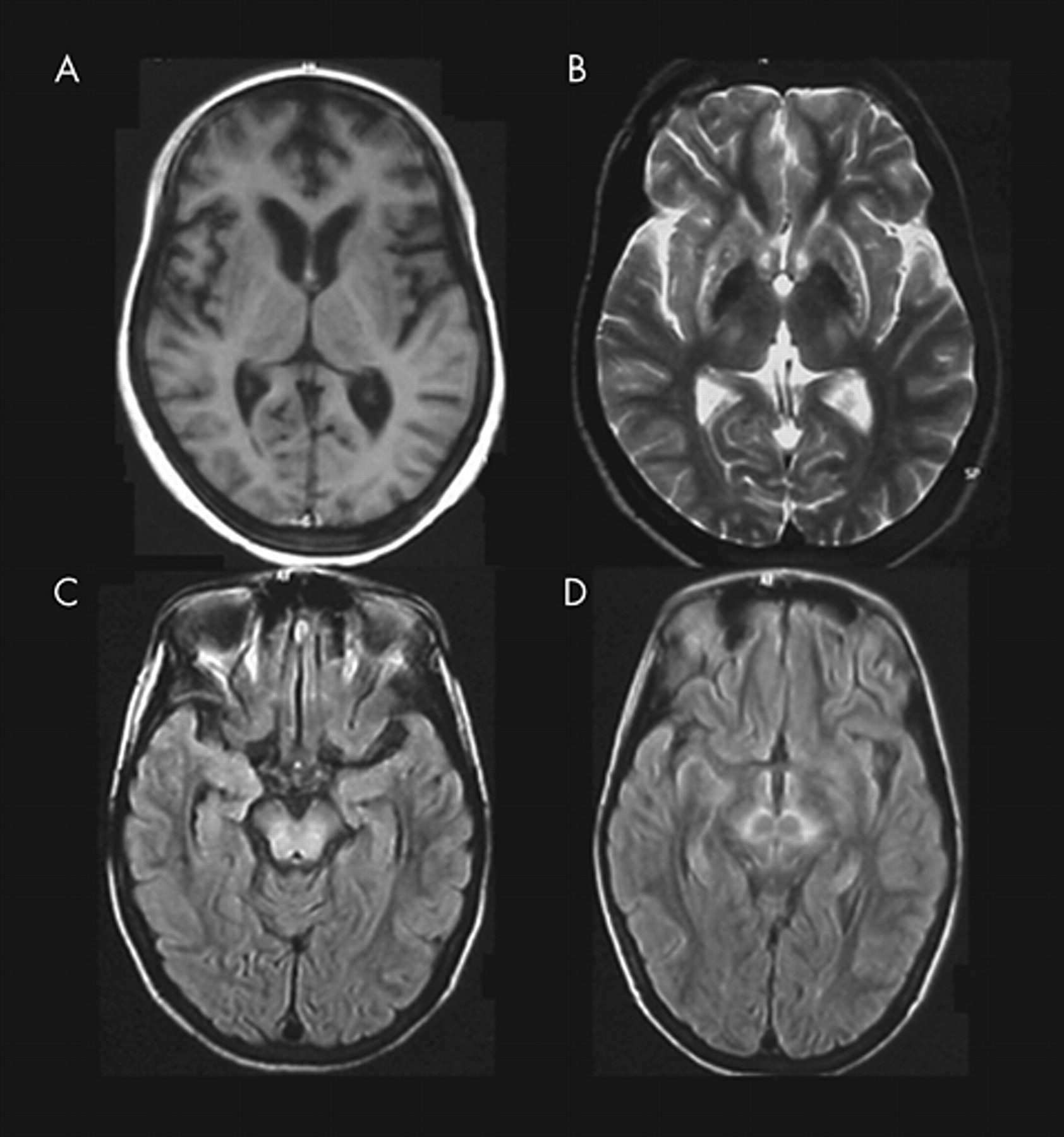
Among these 12 patients, seven had undergone evaluation with magnetic resonance imaging (MRI) of the brain at mean age of 25.4 ± 5.7 years (range: 20–37 years). MRI in these patients showed varied changes. Brain atrophy was noted in five patients, varying from mild to moderate, and included cerebral atrophy (4), brain stem atrophy (4), and cerebellar atrophy (4). Signal intensity changes on MRI were noted in all but one patient and included caudate (3), putamen (5), internal capsule (1), thalamus (4), midbrain (5), pons (3), cerebellum (1), and white matter changes (1) (
Table 2 ) (
Figure 1 ).
DISCUSSION
Dening and Berrios
5 retrospectively assessed 195 patients with Wilson’s disease and observed that 51% displayed psychopathologic features. In another study, Schwartz et al.
6 reported that one third of patients with Wilson’s disease had psychiatric disturbances in the early stage of the disease, and in 20% the psychiatric manifestations preceded all other manifestations. In a prospective study by Akil and Brewer,
2 two thirds of patients with Wilson’s disease had psychiatric symptoms at the time of initial presentation. The present study revealed that 24% (n=12) of patients had psychiatric manifestations and 16% (n=8) of them presented with these symptoms.
The psychiatric manifestations of Wilson’s disease can be categorized into five groups of symptoms: personality changes, affective disorders, psychosis, cognitive impairment, and others.
2 Akil and Brewer
2 believed that behavioral and personality changes and affective disorders, including depression, are the most common psychiatric manifestations of Wilson’s disease. Dening and Berrios
5 noted that schizophrenia-like psychosis, often described in case reports, is infrequent and personality change, depression, and cognitive impairment are common. These often co-occurred with neurological symptoms, but not with hepatic manifestations. Symptoms such as inappropriate behavior and irritability are more often associated with bulbar and dystonic features rather than tremors.
Twenty-four percent (n=12)of patients in this sample fulfilled criteria for syndromic psychiatric diagnosis, 18% (n=9) had bipolar affective disorder, 4% (n=2) were diagnosed with major depression, and 2% (n=1) had dysthymia. Depression was observed in 20%–30% of patients with Wilson’s disease.
2,
5 Other affective disorders such as hypomania and mania, though rare, have also been reported.
2Personality changes in Wilson’s disease include bizarre behavior, impulsivity, occasionally extending to criminal behavior, and disinhibition.
5 Akil and Brewer
2 reported that personality changes occurring as initial manifestations included irritability, emotionality, decreased threshold for anger, and occasional aggression. “Schizophrenia-like” psychosis and other forms of psychosis have been reported infrequently.
5,
7,
8 Psychosis can be an initial manifestation and often leads to an inaccurate diagnosis.
5,
9 Cognitive and intellectual impairment,
10,
11 substance abuse,
12 catatonia,
13 sexual preoccupation,
3 and anxiety disorders
9 have also been reported.
Brain MRI in these patients with psychiatric manifestations revealed changes typically described in patients with Wilson’s disease. Both basal ganglionic and brainstem signal changes were noticed in addition to diffuse atrophy. Keller et al.
14 reported a 38-year-old patient with Wilson’s disease presenting with bipolar affective disorder. The MRI revealed basal ganglia and dorsal midbrain signal changes. Single photon emission computed tomography study with iodine-123-iodobenzamide (IBZM-SPECT) detected a normal distribution of the drug in the brain, with a better signal in the right side and a deficit of D2-dopaminergic receptors in the basal ganglia. The frequency of abnormalities noted in these patients with behavioral changes was not different when compared with a cohort of 100 patients with Wilson’s disease who underwent MRI.
15 Diverse imaging abnormalities have been described in patients with nonorganic bipolar disorder. These include: periventricular and deep subcortical white matter hyperintensities; ventricular enlargement, right more often than the left; decreased volume of subgenual cingular, frontal, and temporal cortices; and morphometric abnormalities in structures such as amygdala, basal ganglia, and thalamus. These abnormalities highlight the role of the fronto-limbic loops involved in the emotion as the pathogenetic mechanism of bipolar disorder.
16 However, the cause and effect relationship of these observations is unclear. Systemic prospective studies of these patients with structural and functional imaging are therefore needed to hypothesize the biological basis of the disease.
The frequency and nature of behavioral and psychiatric abnormalities in Wilson’s disease are variable and attributed to data often being reported by nonpsychiatrists, use of ill-defined terminologies and diagnostic criteria, lack of prospective evaluation, and assessment after regression of symptoms. The current study was designed to explore the psychiatric comorbidity by administering structured clinical interviews in a systematic way.