T raumatic brain injury (TBI) is a growing public health problem with an annual incidence of at least 1.4 million
1 ; of those incidents 75% are mild TBI. While 80%–90% of individuals with mild TBI usually make a good recovery,
2 10%–20% continue to have psychosocial problems, predominantly mood disorder.
3 –
6 Depression is quite common after mild TBI with a prevalence of 15.3%
7 and is a risk factor for poor recovery.
8 –
9 Remarkably enough, mild TBI subjects have
higher rates of depression, postconcussive syndrome, and poor global outcome than those with more severe TBI.
10 There are only a few studies of clinical correlates of mild TBI and depression. Levin et al.
11 reported that risk factors for developing major depression in mild TBI within 3 months of injury include older age and abnormal computerized tomography (CT) scans, with an odds ratio of 7.8 for the latter. To our knowledge, no other studies have looked at preinjury and injury factors associated with the development of depression after mild TBI. This is an important area of study, as identifying people at risk to develop depression soon after the injury can help initiate treatment early on. We present here the preliminary results from an ongoing 1-year longitudinal study examining risk factors for depression after TBI. The current analysis focuses only on risk factors associated with the development of new-onset depression after mild TBI.
Participants and Procedures
Mild TBI patients were recruited from the trauma unit of the Johns Hopkins Hospital and the Brain Injury Unit of Kernan Hospital at the University of Maryland. The study was approved and overseen by the Johns Hopkins Institutional Review Board and the Kernan Hospital Medical Executive Committee. All participants gave written informed consent. All participants received two study evaluations within the first 3 months of the TBI. If participants were able to provide written informed consent within the first 2 weeks of trauma, the first evaluation (V0) was done within the first 2 weeks of TBI (assessing pre-TBI functioning) and the second evaluation (V1) was done around the third month of TBI to assess psychiatric problems and psychosocial functioning soon after TBI. However, for subjects who were unable to give consent within the first 2 weeks of trauma or unable to be contacted, both the pre-TBI (V0) and post-TBI (V1) status were assessed at the time they were contacted and able to provide informed consent, in either the second or third month posttrauma. Follow-up visits were done at 6 and 12 months posttrauma.
Inclusion criteria included (a) first-time closed head injury; (b) clear history of altered mental status or Glasgow Coma Scale (GCS) score less than 15 soon after injury as assessed by the trauma staff or emergency room personnel; (c) admission to the inpatient trauma units for assessment of brain injury; (d) ability to provide consent; and (e) age at least 18 years old.
Exclusion criteria included (a) prior TBI; (b) an open-head injury (e.g., a displaced skull fracture or a gun-shot wound); or (c) history of any other type of brain illness (e.g., stroke, seizure, encephalitis).
As the focus of the analysis is to examine risk factors for new-onset depression after mild TBI, only patients with loss of consciousness less than 30 minutes and no past psychiatric history of mood disorder were included. The results presented here are preliminary and part of an ongoing study on risk factors for depression after TBI of all severities.
Measures
Psychiatric Diagnosis
All participants were interviewed with the Structured Clinical Interview for DSM-IV axis I disorders (SCID-IV). The SCID-IV was administered by a neuropsychiatrist (VR) at each visit. Patients were diagnosed with depression if they met the criteria for mood disorder secondary to general medical condition (TBI), major depressive-like episode, or other depressive symptoms.
Clinical Variables
Demographic information was collected via interviews and review of medical records. Psychosocial functioning was also established using a semistructured interview using the Social Functioning Examination scale and the Social Ties Check List. Scores range from 0.00 to 1.00, with higher values indicating poorer levels of satisfaction. The Family Health Screen was used to collect lifetime psychiatric history of family members. Medical comorbidity was assessed using the General Medical Health Rating scale, a 4-item Likert scale with 4 indicating excellent health and 1 indicating poor health. In addition, the presence of nonhead injuries was captured as presence or absence of body injuries.
Lesion Location
Assessment of lesion location was obtained via CT scans conducted as part of the clinical workup. The CT scans were done soon after injury. For the purpose of this analysis, results were characterized as presence or absence of contusion, intracerebral bleed, subarachnoid hemorrhage, epidural bleed, and subdural bleed in different brain regions grouped as frontal, temporal, parietal, occipital subcortical, and/or cerebellar sites.
Cognitive Tests
The test battery included Mini-Mental State Examination (MMSE); National Adult Reading Test; verbal fluency (letters “s” and “p”) and category (animals and supermarket); Hopkins Verbal Learning Test—Revised; Brief Visuospatial Memory Test—Revised; Trail Making test; Stroop Color and Word Test; Brief Test of Attention, and the Wisconsin Card Sorting Test.
Statistical Methods
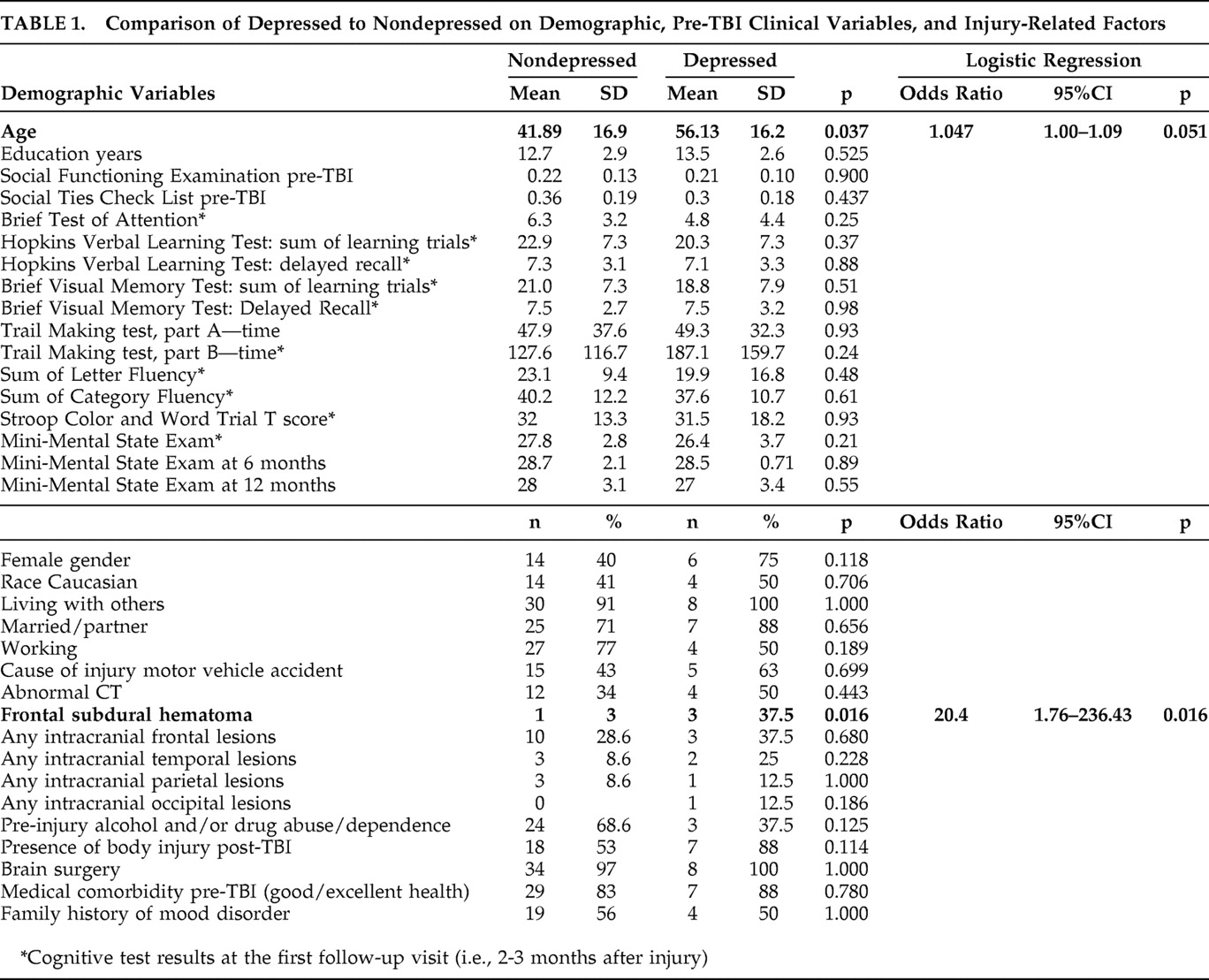
Results were analyzed used a nested case-control design. Cases were patients who were diagnosed with mood disorder due to general medical condition (TBI), major depressive-like episode, or other depressive-symptoms at any time over the follow-up (n=8), while comparison subjects had no depression diagnosis at any time (n=35). None of the cases had a pre-TBI lifetime history of major depression, minor depression, or any other depressive disorder. As there was little difference in results from parametric versus nonparametric tests, parametric tests were chosen. To compare dichotomous diagnostic groups, unpaired t tests were used for continuous variables and Fisher’s exact test for dichotomous variables. The significance level was set a priori at p<0.05. After identifying group differences, logistic regression was used to examine the odds ratio of having a major depression diagnosis for variables that were statistically significant (p=0.05).
RESULTS
Forty-three participants who completed at least one follow-up examination during the 1-year follow-up period were included in the present analysis. The mean age of the sample was 44.5 years old (SD=17.5) and mean education level was 12.9 years (SD=2.9). Fifty-four percent were males (n=23) and 56% were non-Caucasians (n=24). The majority (93%, n=40) lived with family/friends, were either married or had a partner (74%, n=32) and had a full time/part-time job (72%, n=31). Fifty-eight percent had an annual income of 20K or greater (n=25). Motor vehicle accidents were the most common cause (45%, n=20) of TBI, and falls and assaults each accounted for 25% (n=11).
Incidence and Persistence of Post-TBI Depression
Eight of the 43 participants (18.6%) met the diagnostic criterion for mood disorder due to general medical condition (mild TBI) during the first year of trauma. Of these, six participants (75%) met the diagnostic criterion for mood disorder due to general medical condition, major depressive-like episode, and two participants (25%) met criteria for mood disorder due to general medical condition, other depressive symptoms. Of these eight participants who had depression, seven were diagnosed at the first follow-up visit (V1, i.e., 2–3 months after trauma), and one was diagnosed for the first time at the 12 month visit (V12). Of the seven, three were still depressed at the 12 month visit (V12), two were lost to follow-up, one had resolution of depression by the end of 12 months, and the other had not yet completed 1 year.
Comparison of Depressed to Nondepressed Mild TBI Participants ( Table 1 )
The total sample was divided into two groups: those diagnosed with mood disorder due to general medical condition (depressed) at any time over the follow-up and those without (nondepressed). The only significant differences were the greater age and presence of frontal subdural hemorrhage in the depressed group. Lesion laterality could not be analyzed secondary to the small numbers.
The two groups also did not differ on the cognitive tests at any of the follow-up periods. There were no differences in demographic or clinical variables between subjects with minor depression (n=2) and major depression (n=6).
DISCUSSION
Incident depression was found in 18% of patients up to a year after mild TBI. This rate is consistent with Rapoport et al.
7 who found a prevalence of 15% in the first 3 months after a mild TBI. On analysis of demographic variables, most preinjury clinical factors did not differ between depressed and nondepressed participants. The only significant differences were increased age and the presence of frontal subdural lesions in the depressed group. These findings are similar to the study by Levin et al.
11 who found increased age and presence of an abnormal CT scan done soon after mild TBI to predict the development of depression within the first 3 months after a TBI.
The relationship between advanced age and the development of depression after mild TBI is controversial. While our findings support the findings of Levin et al.,
11 Rapoport et al.
12 have found that older mild TBI patients are not at increased risk of developing depression in the immediate trauma period. Our study had longer duration of follow-up (1 year) and included participants with minor as well as major depression, which may be an equally important contributor to morbidity.
13Jorge et al.
14,
15 reported in two studies that major depression post-TBI is associated with left frontal abnormality. Our finding of the positive association between mild TBI depression and frontal subdural hemorrhages supports this association of lesion location with post-TBI depression and extends the results specifically to mild TBI.
Strengths of our study include longitudinal design and use of well-validated psychiatric diagnostic and clinical measures. Limitations include the small sample size, which may have limited identifying other correlates of mild TBI depression, and the absence of more sensitive neuroimaging scans. It is also possible that some patients may have had preexisting microvascular ischemic lesions and executive functioning deficits that may have been misdiagnosed as minor depression. Another limitation is that assessment of pre-TBI status (V0) was done in the first 2 weeks of trauma in only those who could be contacted and/or who provided informed consent within the first 2 weeks of trauma. The rest had their pre-TBI status assessment at 2–3 months post trauma, which could be subject to recall bias.
CONCLUSION
As mild TBI is a growing public health concern and depression after mild TBI a common cause of morbidity, it is important to identify predictors so that treatment interventions can be instituted early on. The results of this study, though preliminary, suggest that there are at least two robust factors (age and frontal subdural lesions) of several possible predictive factors that are associated with mild TBI depression. Emergency room physicians and trauma clinicians can use these results to identify high-risk mild TBI patients and make appropriate referrals.
Acknowledgments
This study was supported by grant K23 MH 066894 from the NIMH. The abstract was presented at the 2008 annual neuropsychiatry conference in Savannah, Ga. Dr. Rao has a grant from Forest to conduct a clinical trial in post-TBI depression and a grant from Pfizer to conduct a clinical trial in poststroke anxiety. Dr. Jason Brandt receives royalties from Psychological Assessment Resources, Inc., on sales of Hopkins Verbal Learning Test and Dr. David Schretlen on sales of Brief Test of Attention. There are no conflicts of interest to declare by other authors on this paper.