Empirical data indicate that people with serious mental illnesses are far more likely to experience traumatic event exposure in their lifetime than those in the general population. Estimates from epidemiological studies indicate that, over a lifetime, traumatic events are experienced by between 36% and 81% of the general population (
1). Comparable rates for people with serious mental illnesses range from 51% to 98%, and the severity and frequency of these traumatic stressors tend to be greater than what the general population experiences (
2). A similar pattern is found for criminal victimization. Teplin and colleagues (
3) found that, during a 12-month period, over one-quarter of persons with serious mental illnesses were victims of a violent crime, a rate that was 11 times higher than that of the general population.
Other research has focused on rates of lifetime and current traumatic event exposure among persons with mental illnesses residing in correctional settings. Not surprisingly, trauma exposure is highly prevalent among people with mental illnesses in correctional settings (
4). Compared with inmates without a mental disorder, those with mental illness were 1.6 or 1.7 times more likely to be physically victimized (male or female inmates, respectively) (
5). Similarly, prevalence rates of sexual victimization among inmates were found to be significantly higher for inmates with a mental disorder than for those without a mental disorder independent of gender, and these rates were higher than those reported for community-based samples (
6).
Lifetime and current rates of physical and sexual assault are likely to be elevated in correctional settings in part because prison environments are violent settings that exploit vulnerable groups (
4), and they disproportionately represent people from socially and economically distressed locations, where rates of violence are typically higher (
3). Incarcerated women report high rates of physical, sexual, or emotional abuse during their formative years and often in adulthood (
7,
8), as well as mental health (
9,
10) and addiction problems (
11). Yet only a small minority of them receive appropriate treatment for behavioral health problems associated with posttraumatic reactions while incarcerated (
12,
13), even though these problems are risk factors for recidivism.
Even though previous studies have documented high prevalence of trauma experiences, very little is known about the details and context of traumatic event exposure history of incarcerated persons and what, if any, associated behavioral health problems these individuals also experience. This information is critically important to the development of integrated treatment interventions designed to address the behavioral health needs of incarcerated persons with mental disorders. Failure to identify and treat trauma-related psychiatric symptoms may result in a range of problematic behaviors, such as substance abuse, interpersonal violence, and gambling, which may lead people back to prison.
The study reported here describes the traumatic event exposure history and behavioral health problems of a sample of incarcerated women who referred themselves to specialty posttraumatic stress disorder (PTSD) treatment. We previously profiled the rates of PTSD and subthreshold PTSD, as well as the associated traumatic events and comorbid psychiatric disorders, among this population (
8). Our goal was to describe the trauma and stress exposure histories of incarcerated women by type of mental disorders (beyond PTSD) in an effort to inform the development of an integrated treatment response to the co-occurrence of trauma, mental disorder, and addiction problems among incarcerated women.
Methods
As part of a parent study to examine a new adapted trauma reentry program in prison, we conducted structured diagnostic clinical interviews and an interview to evaluate lifetime history of traumatic and stressful event exposure with soon-to-be-released female inmates. The purpose of the study reported here was to provide descriptive data on traumatic event exposure history and behavioral health characteristics for this underserved and understudied population.
The study population was English speaking, soon-to-be-released incarcerated women, age 18 years or older, with trauma histories who resided at an adult women's correctional facility (population approximately 850) located in a northeastern state. “Soon-to-be-released” was defined as expected to be released from prison within eight to 36 months from August 1, 2009, and to have at least 30 weeks left to serve at the adult prison. The median term of commitment was five years, with the last 24 months spent in community-based settings for inmates achieving minimum-security status. The study was announced in monthly inmate newsletters and at presentations given in housing units by the investigators. Interested inmates could self-refer for clinical assessment in their housing units, during the orientation presentation, or by sending a note to the study mailbox at the prison.
Of the 418 women who self-referred for screening (roughly half the prison population), 320 satisfied the release date condition (eight to 36 months to release date or to parole eligibility date) to be screened. Overall, ten (3%) of the 320 time-eligible inmates were not screened. Reasons for not being screened varied; four were in administrative segregation, three were in the mental health unit, two signed up after the recruitment interviews were completed, and one was on medical leave. A total of 310 inmates met with a screener. Of those, 97 (31%) either declined to be screened or were determined ineligible at prescreening because they did not have enough time to complete the study, had work conflicts, did not speak English, were unable to participate in the program because of medical limitations, or reported no trauma history. An additional four women were partially screened but did not complete the process because of language barriers or were unexpectedly released to a halfway house. A total of 209 women (mean±SD age 34±9) age 18 or older participated in the full screening: 105 (50%) were African American, 65 (31%) non-Hispanic white, 33 (16%) Hispanic, and six (3%) another race or ethnicity.
Written informed consent was required before study participation. The appropriate university institutional review board and the agency research review committee approved the protocol, recruitment, and consent procedures, as well as the consent form.
Clinical interviews were administered by master's-level, clinically trained social workers or psychologists and were conducted in private rooms. The assessors were trained and supervised by doctorate-level researchers with experience administering these instruments in clinical and research settings related to PTSD and serious mental illnesses (
14). Assessments took approximately two hours to administer. Data were collected from July 2009 through April 2010.
The clinical interview included the following instruments: the Clinician-Administered PTSD Scale (CAPS), to diagnosis lifetime and current full or subthreshold PTSD; the Structured Clinical Interview for DSM-IV Non-patient Version (SCID-NP), to assess other axis I disorders, including alcohol and substance abuse or dependence disorder; and the Trauma History Questionnaire and the Life Stressor Checklist-Revised (LSC-R), to assess trauma history. All clinical measures are commonly used with traumatized populations and were scored in standard fashion.
Diagnostically, full PTSD was defined as having a qualifying traumatic event, one reexperiencing symptom, three avoidance symptoms, and two arousal symptoms with the presence of co-occurring significant distress and impairment. Subthreshold PTSD classification required a qualifying traumatic event, one reexperiencing symptom, and either three avoidance or two arousal symptoms with the presence of co-occurring significant distress and impairment (
15).
Respondents were classified into groups according to mental disorder status (serious mental disorder, other axis I disorder, or no axis I disorder) for both descriptive and comparative purposes. Serious mental illness includes psychotic disorders, bipolar disorder, and major depressive disorder. Other axis I disorder includes anxiety disorder, dysthymic disorder, depressive disorder, and other mood disorder. The significance levels used to assess the validity of the null hypotheses were p<.05 and p<.01. Means and percentages were estimated on the basis of valid numbers. SAS 9.2 was used for the analysis, and Proc means and freq were used to construct all statistics. Given the small sample size and the exploratory nature of the study, Bonferroni-type alpha adjustments were not conducted, which raised the possibility of type I error but minimized type II error.
Results
On average, the 209 incarcerated women who self-referred to trauma treatment were 34 years old and serving time for a violent crime, and a large majority had an axis I psychiatric disorder (178 of 209, 85%), symptoms that met the criteria for full or subthreshold PTSD (N=184, 88%), and substance abuse or dependence problems (N=181, 87%). Women with an axis I disorder were significantly and substantially more likely to have full PTSD than their counterparts without an axis I disorder (83% versus 42%). [Tables providing further details are provided in an online supplement to this brief report at
ps.psychiatryonline.org.]
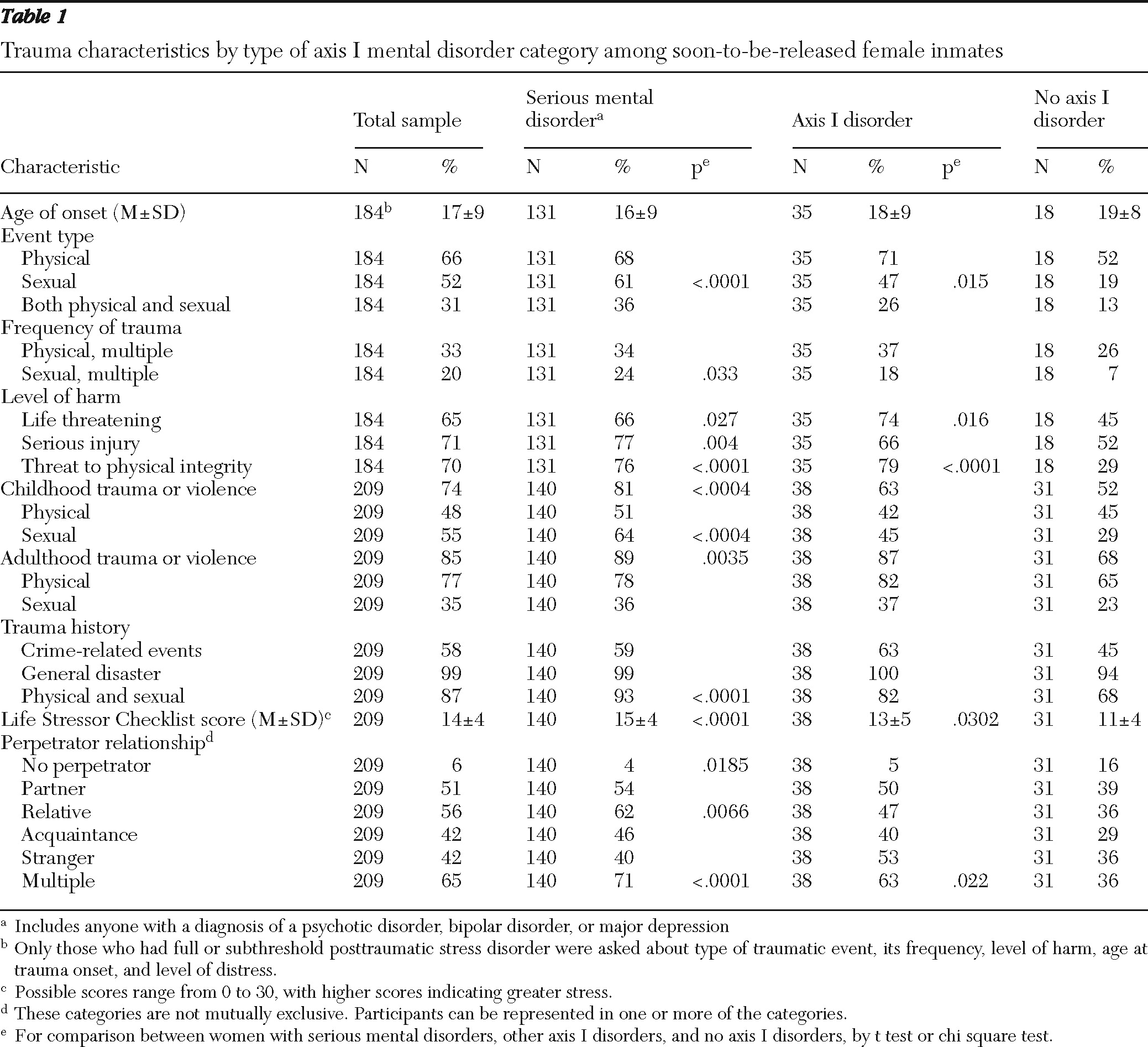
Traumatic event exposure was highly prevalent (
Table 1). More than 50% of the incarcerated women reported experiencing at least one event of physical or sexual abuse perpetrated by someone they knew; the abuse was life or physically threatening and resulted in severe to extreme distress. Nearly three-quarters or more of the women reported childhood trauma (physical or sexual) and adult physical trauma. Rates of childhood and adult interpersonal trauma were highest among incarcerated women with a serious mental disorder (81% and 89%, respectively). Women with a serious mental disorder were most likely to report experiences of sexual abuse.
Obtained data also profiled the lifetime traumatic and stressful event histories of these incarcerated women (
Table 1). Majorities of the sample reported experiencing at least one type of crime-related (58%), general disaster-related (99%), or interpersonal (87%) trauma. These types of trauma were least likely to be reported by women with no axis I disorder. Of the women with a serious mental disorder, over 60% reported that at some point in their lives they feared being killed or injured, saw someone injured or killed, had someone close to them become seriously injured or die, experienced abusive sexual contact, or were forced to have sex against their will. Mean scores on the LSC-R were significantly higher for women with a psychiatric disorder compared with women with no psychiatric disorder. Compared with women without an axis I disorder, women with a serious mental disorder were more likely to report experiencing foster care or adoption, serious money problems, serious physical or mental illness, emotional abuse or neglect, and some form of abuse both before and after age 16. [See online supplement for details.]
Discussion
Data from this large typical sample of treatment-seeking, soon-to-be-released female inmates revealed high rates of serious mental illness (67%), with only a small percentage (15%) of the sample exhibiting no axis I psychiatric disorder; presence of psychiatric disorders, especially those classified as serious mental illnesses, were significantly associated with a history of traumatic event exposure, especially interpersonal violence and full or subthreshold PTSD; significant and complex histories of traumatic event exposure, including high rates of overall traumatic event exposure (88%) and childhood sexual or physical trauma (74%); and descriptive profiles of specific lifetime traumatic and stressful event experiences associated with serious mental disorder and other psychiatric disorders. Together, these findings suggest strong behavioral effects associated with lifetime traumatic and stressful event histories and clearly indicate major behavioral health care needs among female prison inmates that are likely unmet by currently available services.
The lifetime traumatic event histories of our sample were characterized by multiple, complex, and severe episodes of interpersonal physical and sexual violence in both childhood and adulthood. Most of the sample reported at least one significant lifetime traumatic event, and about two-thirds reported a traumatic event that was perceived as life threatening and that actually caused serious physical injury. Both physical and sexual interpersonal violence were common, and 30% of the sample reported experiencing both at some point in their life. Moreover, traumatic events occurred throughout the life span. Childhood violence was experienced by over 70% of the sample, with a majority (55%) reporting sexual violence. Of the 85% reporting traumatic experiences during adulthood, physical violence was most frequent (77%), and sexual violence (35%) was common. Perpetrators of this violence were spread rather evenly across partners, relatives, acquaintances, and strangers. Over half of the sample (65%) reported experiencing interpersonal violence from more than one perpetrator. Frequency of individual types of traumatic and stressful life experiences was significantly higher in the serious mental disorder group than among participants with no psychiatric disorder.
In addition to all the usual methodological limitations of cross-sectional and self-report research, this study had several additional limitations. First, it included only female inmates who were self-referred for inclusion in an intervention that focused on addressing PTSD, other posttraumatic reactions, and reentry preparation. Participation was limited to women who spoke English and were soon to be released. Thus findings may not generalize to the female prison population as a whole. This concern is mitigated somewhat by the fact that approximately a quarter of the total prison population was fully screened for participation. Most of the potential participants who satisfied the release date condition participated, and even the most conservative interpretation of the data indicate high levels of serious mental disorder, PTSD, and traumatic and stressful event exposure. Second, self-report histories regarding potentially threatening topics (trauma and psychopathology, for example) by vulnerable people (inmates) are subject to a variety of errors and respondent biases beyond mere faulty recall. Third, our structured clinical interviews did not include reliability checks beyond rigorous training and supervision procedures. Concern about these study limitations is mitigated by the study's strengths, including a large typical sample of female inmates and a group whose behavioral health care needs are vastly understudied. In addition, the use of structured clinical and diagnostic interviews, conducted with careful training and supervision, also represent a strength of this study.
Conclusions
These findings identify prominent behavioral health care needs within a particular section of the female inmate population and are suggestive of the general level of need within the broader female prison population. Female inmates appeared to have extensive lifetime traumatic and stressful event exposure histories and met DSM-IV criteria for multiple psychiatric disorders, including serious mental illnesses, PTSD, and past substance use disorders. Identifying trauma exposure, especially interpersonal trauma, within this population and providing effective interventions hold promise for preparing incarcerated women to better manage their lives in ways that will keep them safe, healthy, and in the community after release from prison.
Future controlled research is needed with this population and with male inmates in regard to optimal strategies for screening and treating trauma-related psychopathology. Research needs to address not only how to most effectively treat posttraumatic psychopathology but when and how best to integrate it with other medical and reentry services. In fact, fragmentation of these various services represents a significant barrier to maximizing care for inmates. Commonly used medications (antipsychotics) may be problematic or ineffective, whereas trauma-focused psychotherapy (exposure) may not be appropriate for people who are living in stressful or traumatic environments. This will require careful consideration in the design and implementation of treatment efforts. Ultimately, research is needed to examine optimal ways of integrating trauma-informed medical and mental health services with community reentry programs.
Acknowledgments and disclosures
This study was supported by grant OJP-2008-MO-BX-0004 from the Office of Justice Programs and by grants P20-MH66170 and P30-MH079920 from the National Institute of Mental Health.
The authors report no competing interests.