Patients with borderline personality disorder place a high demand on health and social services
(1). In our recent randomized controlled trial comparing partial hospital treatment of borderline personality disorder with treatment as usual, we found a favorable outcome on symptomatic and clinical measures for the partial hospital treatment group both at the end of treatment
(2) and after 18 months of follow up
(3). This article reports a cost analysis of the data from the trial, focusing on the direct costs of partial hospital treatment compared with treatment as usual and on subsequent use of services over 18 months for all patients.
Method
The design of the study, the sample characteristics and criteria used for borderline personality disorder, and the written informed consent obtained after explanation of the procedure have been detailed in an earlier publication
(2). For this report, information about service utilization in the 6 months before point of randomization, during the 18 months of the study, and over the course of the 18-month follow-up period was collected from case records of the 22 patients (including dropouts) in the partial hospitalization group and the 19 patients in the general psychiatric care group who participated in the original study. Case records include mental and physical health provision for patients but do not include social and other government services provided. Mental health provision was relatively easy to monitor and cost, since all patients were treated in local facilities because of the contracted nature of the service. Records of all relevant services were searched for the patient’s unique NHS (social security) numbers. The services monitored included psychiatric inpatient treatment (days), outpatient visits (number), partial hospital treatment (weeks), community-based mental health services, and types and duration of pharmacological treatments (weeks of antidepressant and antipsychotic medication, minor tranquilizers, and mood stabilizers), and general hospital casualty visits (number).
Case notes were scrutinized by two coders and compared with service utilization data obtained independently from the service providers. Prescribing patterns were monitored from prescription charts and dispensing records. Reliability of coding was high (98% agreement between coders), but confirmation from independent sources generated minor discrepancies, particularly concerning exact dates of admission or discharge, the nature of medical interventions, pharmacotherapy, and the type of community support offered. Where disagreements were identified, an independent rater blind to treatment condition was asked to arbitrate. Use of community-based services (e.g., specialist drug and alcohol services) was not possible to ascertain reliably from the records until the follow-up period. Since only the general psychiatric care group was in receipt of these services during the treatment period, excluding their costs for both groups reduces the likelihood of finding differences favorable to the experimental group.
Services provided were costed at published local rates. These include “hotel” and staffing costs of each individual facility or activity, giving a unit cost for each activity. The cost of drugs was based on the contracted hospital price.
Service usage included many combinations and could be meaningfully contrasted across the two groups in terms of the cost of different treatments. We considered three cost categories: 1) psychiatric care that included the total cost of inpatient, outpatient, and partial hospital treatment services used by the patient; 2) pharmacological treatment cost; and 3) general hospital costs related to interventions in emergency rooms.
All analyses were carried out by using SPSS for Windows (Version 10). Total costs incurred for psychiatric (inpatient, outpatient, partial hospital treatment), medication, and emergency room treatment were calculated for each patient for each 6-month period, and these values were averaged for the 18 months of treatment and the 18 months of follow-up. All costs were expressed as estimated annual costs in U.S. dollars (£1=$1.41). We used nonparametric statistics throughout because of the highly skewed distribution of the cost data. The partial hospitalization and general psychiatric care groups were contrasted at pretreatment, treatment, and follow-up by using Mann-Whitney U tests. The statistical significance of changes between pretreatment, treatment, and follow-up within groups was determined by using Wilcoxon signed ranks test. Because no figures were available for the cost of community support during pretreatment and treatment, cost comparisons within groups across time were made only for inpatient, outpatient, medication, and emergency room treatment.
Results
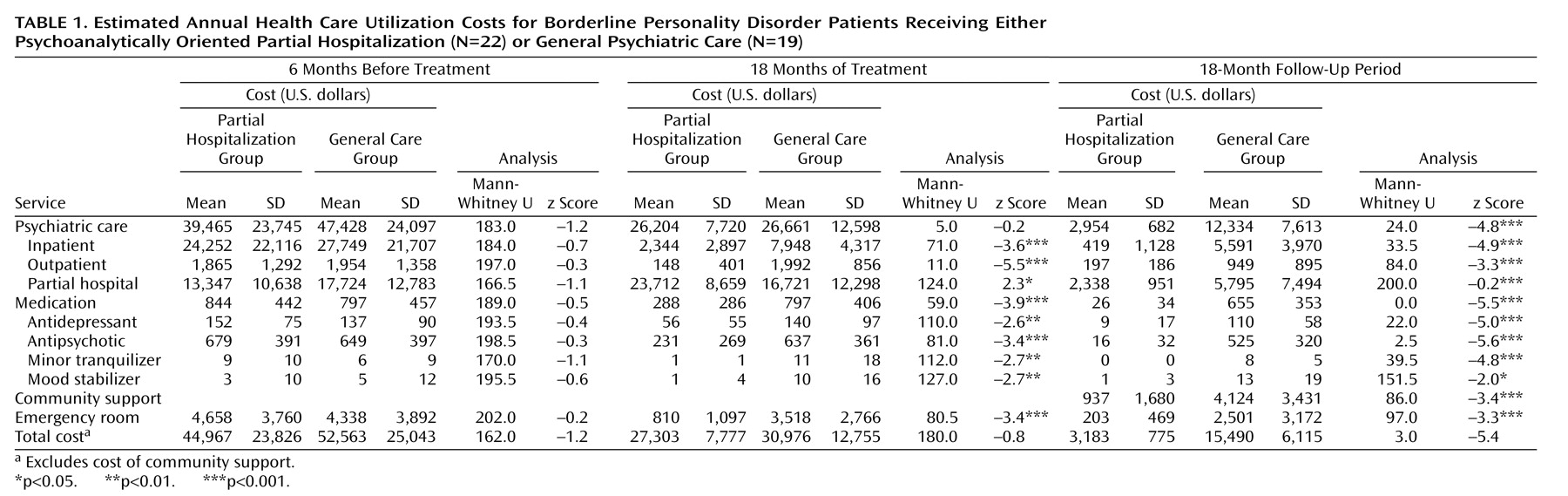
Results are summarized in
Table 1. The two groups were similar in terms of health-related costs before treatment. During treatment, the overall costs remained comparable; the higher partial hospital treatment costs for the partial hospitalization group were offset by lower costs of inpatient and outpatient care, medication, or emergency room treatments. For the 18-month treatment period, Wilcoxon tests showed that estimated annual costs were significantly lower for both the partial hospitalization group (z=–3.1, p<0.002) and the general psychiatric care group (z=–3.0, p<0.003) compared with the 6-month pretreatment costs. This was due to substantial reductions in the costs of inpatient and outpatient psychiatric care in the partial hospital treatment group (z=–4.1 and –4.0, respectively; p<0.001) and the reduction of inpatient care for the general psychiatric care group (z=–3.3, p<0.001). The cost of medication and emergency room care decreased significantly only in the partial hospitalization group (z=–3.9 and –4.0, respectively; p<0.001).
Costs diverged sharply following discharge. The average annual cost of monitored health care for the partial hospitalization group was one-fifth of that for the general psychiatric care group. Differences were marked in all the monitored domains of care, including the costs of community support. Notably, these costs represented significant reductions in psychiatric treatment (partial hospitalization: z=–4.1, p<0.001; general psychiatric care: z=3.1, p<0.002) and medication costs (partial hospitalization: z=–4.0, p<0.001; general psychiatric care: z=–2.2, p<0.03). But while the total cost was significantly reduced during follow-up for both groups (partial hospitalization: z=–4.1, p<001; general psychiatric care: z=–3.2, p<0.001) only the partial hospitalization group showed a significant reduction in emergency room costs relative to the treatment period (z=–2.8, p<0.005).
Discussion
This study indicates that there are considerable savings to be made over time by providing a specialist partial hospital treatment service for patients with borderline personality disorder rather than offering treatment as usual. While the partial hospital treatment program itself is an additional cost, this is offset even during treatment by a reduction of inpatient and emergency room treatment. At follow-up, compared with pretreatment costs, the mean annual cost savings associated with the program were $12,000, thereby recouping the cost of the program over 2 years.
There are a number of major limitations to this study, including the small study group size, the limitations to the randomization (three excluded subjects in the general psychiatric care group crossed over and three early dropouts from partial hospital treatment group) and the multicomponent treatment package. We have partially addressed these limitations by including data from early dropouts in an intent-to-treat analysis and by manualizing the treatment package. Our inability to cost adequately community support over the course of treatment and estimate indirect costs further limits generalization. Costs based on U.K. statutory service provision might not match those of other countries. Nevertheless, this study suggests that the favorable outcome of a psychoanalytically oriented partial hospital treatment program for borderline personality disorder is cost effective.